 |
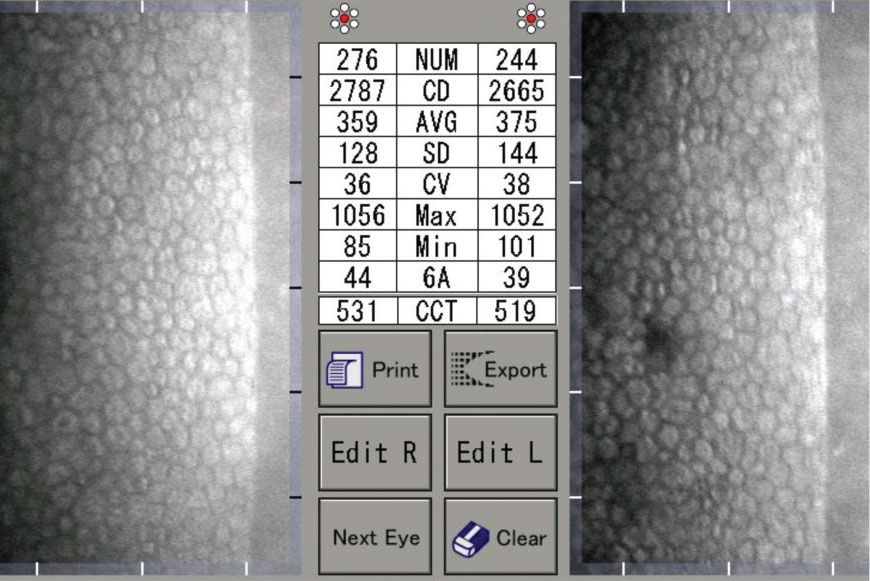
| Both patients with type 1 and type 2 diabetes both experience a decrease in endothelial cell density. Photo: Daniel Epshtein, OD. Click image to enlarge. |
Diabetic retinopathy isn’t the only ocular complication that people with diabetes may experience. Corneal abnormalities often predispose these patients to recurrent corneal erosions and reduced corneal sensitivity. According to animal models and laboratory studies, corneal endothelial cells undergo metabolic dysfunction in diabetic conditions. Corneal endothelial compromise in diabetic patients hasn’t been well-studied, but a recently published study in Cornea found that both type 1 and type 2 diabetes reduce corneal endothelial cell density and increase pachymetry.
The literature search identified 752 records, 17 of which met inclusion criteria. The team evaluated the role of both types of diabetes on corneal endothelial cell density and pachymetry. Age was one of the modulators the researchers used to differentiate between normal age-related changes and diabetes and to assess the impact of disease duration.
The researchers reported that patients with type 1 diabetes had an average of 193 cells/mm2 fewer than control patients and patients with type 2 diabetes had an average of 151 cells/mm2 fewer than controls. Patient ages were similar among controls and those with type 1 and type 2 diabetes in the study, so loss of corneal endothelial cells was expected. However, those with diabetes demonstrated increased pachymetry compared with control patients, and in both types 1 and 2 diabetes, increased pachymetry was associated with disease duration.
“This study adds to the available knowledge by making an independent estimation of corneal endothelial cell density and pachymetry for each type of diabetes and by including the mean age in the model of evaluation,” the researchers noted. “This helps us to understand the impact of the disease considering the reduction in corneal endothelial cell density expected over time and the increase in pachymetry at different ages. Our analysis demonstrated that diabetes mellitus types 1 and 2 are associated with reduced corneal endothelial cell density and increased pachymetry. These differences were bigger between patients with type 2 diabetes and controls, independently of the reduction in the endothelial cell density and the increase of pachymetry expected by the normal aging process.”
The researchers explained that the main factors associated with corneal endothelial pathophysiology in diabetes patients are a high glycemic environment and reduced or null amount of insulin. With excess glucose, corneal endothelial cells—whose glucose entry doesn’t depend on insulin—are exposed to the task of modulating entry of glucose and become prone to complications.
“It’s interesting that a significant relation between the duration of the diabetes mellitus and the progressive reduction in corneal endothelial cell density was only found in the type 2 diabetes group; whereas, for both types of diabetes, the central corneal thickness correlated with the duration of the disease,” they noted. “Moreover, the calculated rate of central corneal thickness change was very similar in both types of diabetes. Overall, these findings point out that there must be a pathophysiological mechanism associated with type 1 diabetes that affects the corneal endothelial cells and isn’t correlated with duration of the disease.”
The researchers said that the meta-regression model they used offered a more accurate estimation of the association of each type of diabetes and reduction in corneal endothelial cell density or increase in central corneal thickness. They concluded, “This confirms that each type of diabetes and the duration of disease contribute differently to corneal endothelial compromise, and this clinically requires further attention.”
Amador-Muñoz DP, Conforti V, Matheus LM, et al. Diabetes mellitus type 1 has a higher impact on corneal endothelial cell density and pachymetry than diabetes mellitus type 2, independent of age: a meta-regression model. Cornea. 2021;1-9. |

