 |
Q:
I have a patient who recently had neurosurgery for an acoustic neuroma and now has facial nerve palsy and a persistent epithelial defect. Until he sees an oculoplastic specialist, how can I preserve the corneal surface and help the persistent defect heal to prevent infection?
A:
These patients can be problematic because they usually have a neurotrophic cornea and an exposed ocular surface, according to Christopher J. Rapuano, MD, chief of the cornea service at Wills Eye Hospital. He says the goal is to keep the corneal epithelium intact in an effort to prevent ulceration, infection, scarring, melting and perforation. Though doctors can accomplish this task in several ways, Dr. Rapuano notes that “the specific approach usually depends on the health of the corneal surface.”
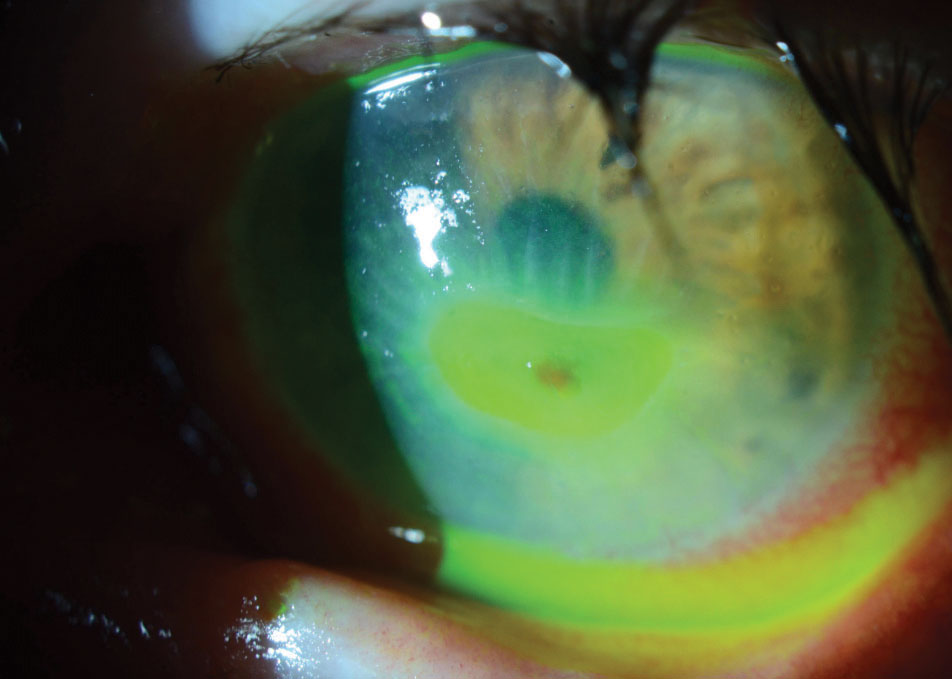 |
This corneal melt developed in an eye with a neurotrophic cornea after undergoing acoustic neuroma treatment. |
A Case-by-case Basis
While Dr. Rapuano says mild cases may respond to simple solutions, such as preservative-free tears four to six times per day and tear gel at night, most cases require more aggressive treatment. He suggests using a viscous lubricant during the day—such as a thick, preservative-free artificial tear—and an artificial tear ointment at night.
In the case of an epithelial defect, Dr. Rapuano recommends using a broad-spectrum antibiotic drop three to four times per day and an artificial tear ointment or an antibiotic ointment every two hours while the patient is awake.
If a patient has a persistent epithelial defect like this patient, Dr. Rapuano notes that a bandage soft contact lens (BSCL) may be necessary but could increase the risk of infectious keratitis. He says the next step is to apply a self-retained amniotic membrane, which can be attached to a plastic ring or placed under a BSCL. The amniotic membrane tends to be quite successful in treating persistent epithelial defects and eventually dissolves over a period of days or weeks, Dr. Rapuano adds.
The doctor’s course of action following treatment for the persistent epithelial defect depends on whether the defect responds positively. If it only responds partially to treatment, Dr. Rapuano recommends applying another amniotic membrane. However, if the defect does not respond, and especially if the cornea begins to thin, he suggests referring to a corneal specialist for more aggressive treatment.
An additional option includes securing the amniotic membrane tissue to the cornea with sutures and/or fibrin glue. He adds that using cyanoacrylate glue may be helpful when trying to avoid an urgent corneal transplant if severe corneal thinning, a descemetocele or a small corneal perforation is present.
Prior to a more permanent eye closure by an oculoplastic surgeon, Dr. Rapuano suggests simply taping the eye closed at night using external aides, such as nasal strips, which are gentle on the patient’s skin. He says some doctors go as far as applying superglue to the eyelashes to glue the eye shut. This can be dangerous, however, and he encourages doctors to exercise caution and carefully use the glue to avoid touching the globe and causing significant corneal and conjunctival damage.
While doctors can attempt to heal the defect, Dr. Rapuano says at the end of the day, “the best solution is closure of the eyelids by an oculoplastic surgeon.”

