New research on bacterial resistance rates to antibiotics offered some surprising findings at this years Association for Research in Vision Ophthalmology (ARVO) meeting.
Other corneal studies focused on the effects of graft-versus-host disease, diffuse lamellar keratitis and herpetic keratitis.
Researchers also introduced new theories on treating dry eye and keratoconus. And, of course, contact lens wear was given its due, with both bad and good news for orthokeratology proponents.
Resistance Rates Climb
Second-generation fluoroquinolones still offer a broad range of coverage in patients with bacterial keratitis.
Researchers continue to track the ever-changing rates of bacterial resistance to antibiotics. An in vitro French study looked at antibiotic susceptibility of isolates recovered from bacterial keratitis patients. The researchers found that second-generation fluoroquinolones still offer a broad range of coverage.4918 Ofloxacin killed 100% of the Staphylococcus isolates, and ciprofloxacin killed 97% of the Gram-negative isolates. Older agents such as gentamicin and rifamycin killed 92% and 91% of Staphylococcus isolates, respectively.
Methicillin-resistant Staphylococcus aureus (MRSA) is emerging as a dangerous pathogen, concludes a multi-center U.S. study.4924 Overall in vitro resistance rates to 30 MRSA isolates were: moxifloxacin, 74%; gatifloxacin, 77%; ciprofloxacin, 91%; and ofloxacin 91%. This came as a surprise to the researchers since most Gram-positive isolates are susceptible to fourth-generation fluoroquinolones.
The newer fluoroquinolones performed better against Pseudomonas aeruginosa in a Mount Sinai Medical Center study, although this bacterium seems to be gaining strength as well.4922 The majority of isolates were susceptible to these drugs, but significant numbers of those collected were resistant: levofloxacin, 25%; moxifloxacin, 28%; and gatifloxacin, 21%.
Microbacterial growth does not pose a threat to antibiotic bottles, regardless of whether the preservative benzalkonium chloride (BAK) is present, concludes a study from New York Eye and Ear Infirmary.4912 The study looked at 100 bottles of gatifloxacin, which contains BAK, and 100 bottles of moxifloxacin, which does not. Only one bottle of moxifloxacin tested positive for coagulase-negative Staphylococcus, but researchers concluded that this was not statistically significant.
Protection from Inflammation
Chronic graft-versus-host disease (GVH) is a well-known cause of ocular surface disorders such as dry eye. However, a French study concluded that transplant patients who successfully avoid GVH may still be at risk for corneal problems.133 Researchers evaluated 14 healthy patients and 11 patients who recently underwent successful bone marrow transplants. Transplant patients scored lower on Schirmers tests and ocular surface quality-of-life assessments. They also had higher discomfort levels and more dry eye symptoms. Levels of inflammatory markers such as trefoil factor 1 (TFF1) were also higher in transplant patients.
Animal model research performed by teams of scientists at the Institute of Ophthalmology and Visual Science in Newark, N.J., and the Sloan-Kettering Cancer Center, in New York, may offer a model of late-onset diffuse lamellar keratitis (DLK).129 Researchers created corneal flaps in eight eyes of four rabbits and intentionally damaged one eye of each rabbit with chemical or mechanical injury. Histopathological analysis showed an inflammatory response in the damaged eyes, with focal aggregates of heterophils, macrophages and mild corneal edema at the flap-stromal interface.
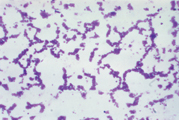
Staphylococcus isolates. Gentamycin and rifamycin each killed more than 90%.
Another animal study provided positive data on a new agent that could be used to treat dry eye and chronic superficial keratitis (CSK).131 Twelve dogs with dry eye and 17 with CSK underwent treatment with pimecrolimus, an ascomycin derivative that inhibits the production of inflammatory cytokines. Researchers gave the dogs one drop of 1% pimecrolimus solution tid. The treatment success was pronounced or moderate in nine of the dogs with dry eye and 14 of the dogs with CSK.
Researchers suggested the agent may help treat dry eye in humans.
Preliminary results from the Herpetic Keratitis and Atopic Disease Study (HADS) indicate that patients with allergies do not experience increased rates of recurrence for herpetic keratitis.118 Researchers divided 58 eyes of 50 patients with herpetic keratitis into two groups: those with a history of atopic disease and those without. Though atopic patients showed a higher recurrence rate, it was not statistically significant.
Researchers have always suspected that coexisting neurotrophic keratitis (NTK) causes the highly destructive nature of methamphetamine keratitis (MAK). Now, a team at Loma Linda University in Loma Linda, Calif., and and Doheny Eye Institute, Los Angeles, has lent credence to that theory.103 A 36-year-old homeless man with an admitted history of methamphetamine abuse was admitted for treatment of a severe Pseudomonas corneal ulcer. He was the first ever documented MAK case with associated NTK.
Researchers at the University of Texas Science Center in San Antonio compared two antifungal agentsthe new micafungin and the traditional natamycinand found little difference between the two.113 They inoculated 16 rabbit eyes to form corneal infiltrates and split them into three groups: untreated, micafungin-treated and natamycin-treated. The only statistically significant difference between the two agents was in hypopyon height, which was significantly lower in the micafungin-treated group.
Dry Eye Etiology
Research continues to offer information on the roots of dry eye syndrome. Spurred by recent studies that link Helicobacter pylori (HP) to Sjgrens syndrome, a German investigation found that patients with this bacterial infection exhibited increased symptoms of ocular dryness.3903 Researchers looked at 53 patients (33 who tested negative for HP and 20 who tested positive). The HP patients showed reduced volume on Schirmers tests, suggesting that eradication of the bacteria could reduce symptoms.
A team of scientists at the Juntendo University School of Medicine in Tokyo and LSU Eye Center in New Orleans found that ocular dryness may cause increased growth of the accessory lacrimal gland on the tarsal conjunctiva.63 They discovered the additional lacrimal gland tissue in dry eye rabbit models.
In recent years, scientists have discussed the main lacrimal gland and the interconnecting neural reflex loops that compromise a functional unit. Studies have linked dry eye with an alteration in corneal innervation due to diabetes mellitus, contact lens use and LASIK. A team of Spanish researchers found that patients with dry eye secondary to Sjgrens syndrome as well as patients with non-Sjgrens syndrome dry eye also exhibited abnormalities in corneal innervation.3891
Novel Keratoconus Treatment
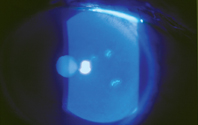
Wavefront technology can help practitioners differentiate keratoconus (KCN) and pellucid marginal degeneration (PMD) from symmetric or regular astigmatism, according to a study team at the Pepose Vision Institute in Chesterfield, Mo.2893 Researchers performed wavefront evaluations on six normal, 19 keratoconic and three PMD eyes. The diseased eyes exhibited inferior corneal thinning and steepening that caused coma-like and trefoil-like aberrations. Vertical coma was increased significantly in keratoconic eyes but not in PMD eyes, and vertical trefoil was selectively increased in PMD eyes.
Once keratoconus is diagnosed, a German study presented a surgical alternative for the 20% of keratoconus patients who will eventually require penetrating keratoplasty.2887 Riboflavin/ultraviolet-A-induced collagen crosslinking, a new procedure, removes corneal epithelium by applying photosensitizing riboflavin drops and exposing the cornea to UVA light for 30 minutes. Animal models have shown an increase in corneal biomechanical stiffness after the treatment.

Wavefront technology can help distinguish keratoconus, as seen here, from symmetric or regular astigmatism.
Researchers at the University Eye Clinic in Dresden performed the procedure on 60 eyes of 40 patients suffering from progressive keratoconus who had moderate or advanced keratectasia. None of the treated eyes exhibited progression of K-readings. The researchers found a postoperative regression of K-readings in 31 eyes with an average reduction of 2.87D. In 38 months of follow-up, no negative side effects were observed.
Ortho-K Revisited
Two rabbit studies conducted at the University of Texas offer good and bad news for the future of orthokeratology.1535,1582 The good news: Reverse-geometry ortho-K lenses do what their makers claim they do, namely compress the central corneal epithelial cells, flattening them in lateral directions. Twelve rabbits were fitted with orthokeratology lenses or gas permeable controls. Central cell size increased 29% for the ortho-K eyes and 5.3% for the RGP eyes. This suggests that the cells are being compressed more with the ortho-K lenses.
The bad news: Ortho-K lenses appear to cause increased binding of Pseudomonas aeruginosa to rabbit corneas when compared with the gas permeable controls, even though both lenses were made from the same hyper-O2 material. Studies are needed to see if this increase in binding occurs in humans, the researchers suggested.
More evidence that long hours of daily soft contact lens wear puts patients at risk for pannus was produced by a study at the University of California, San Francisco.1560 Researchers evaluated the tears of three groupsa control group, occasional soft contact lens wearers (one to three days a week) and chronic wearers (12 hours daily)for levels of vascular endothelial growth factor (VEGF). This mediator is stimulated in response to hypoxia and inflammation. Mean VEGF level was 307pg/ml in the tears of controls, 383pg/ml in occasional wearers was and 636pg/ml in chronic wearers.
Short-term application of multipurpose contact lens solutions does not damage corneal cells, according to a University of Houston study.1533 Researchers looked at eight neophyte subjects who received either one-day applications of MPS-A, containing polydronium hydrochloride, or MPS-B, containing poloxamine. The contralateral control eyes received non-preserved saline solution. They then compared corneal basal epithelial cell numbers in vivo using a ConfoScan 3 confocal microscope. Neither multi-purpose solution showed evidence of acute increase in corneal exfoliation or damage when compared with the saline controls.
63. Toshida H, Murakami A, Nguyen DH, et al. Three-dimensional analysis of accessory lacrimal gland in a rabbit model of dry eye.
103. Kroll MA, Affeldt JC, Hayes J, Meallet M. Methamphetamine keratitis as a variant of neurotrophic ocular surface disease.
113. Trujillo F, Paris G, Woodward L, et al. Comparison of two antifungal agents, natamycin and micafungin, for fungal keratitis.
118. Rezende R, Freitas JB, Hammersmith K, et al. Evaluation of the severity of herpetic keratitis in the atopic patients.
129. Chu DS, Ayres BD, La Perle K, Hersh PS. Inflammatory response at the corneal flap-stromal interface after mechanical and chemical injuries in white New Zealand rabbit corneas.
131. Nell B, Walde I, Spiess BM, et al. Exploratory study reveals topical pimecrolimus is active against keratoconjunctivitis sicca and chronic superficial keratitis in dogs.
133. Lafontaine PO, Brignolle-Baudouin F, Buron N, et al. Assessment of ocular surface during graft versus host disease. Clinical and biological assessment of clinical score such as Schirmer 1, Schirmer 2, BUT and patient subjective discomfort, and biological peptide secretion of HLA-DR, MUC5AC and TFF1.
1533. Wang Q, Guerra J, Bergmanson J, Miller W. The effect of multipurpose solutions on human cornea cells under in vivo confocal microscope.
1535. Ladage PM, Yamamoto N, Cavanagh HD. Confocal microscopy of the rabbit corneal surface following orthokeratology lens wear.
1560. Magone T, Strauss EC, Francis I. VEGF levels in the tears of soft contact lens wearers.
1582. Yamamoto N, Ladage PM, Cavanagh HD. Pseudomonas aeruginosa binding to the rabbit corneal surface following orthokeratology lens wear.
2887. Sandner D, Spori E, Kohlhaas M, et al. Collagen crosslinking by combined riboflavin/ultraviolet-A (UVA) treatment can stop the progression of keratoconus.
2893. Pepose J. Pepose J. Wavefront aberrations in patients with keratoconus and pellucid marginal degeneration.
3891. Benitez Del Castillo JM, Wasfy M, Martinez-de-la-Casa JM, et al. Masked study of corneal nerves in dry eye patients using confocal microscopy. 3903. Blomberg L, Hauschild S, Gockein R, Brewitt H. The dry eye syndrome and the gastral Helicobacter pylori infection: Pilot study about a possible existing epidemiological relationship.
4912. Kaiura TL, Ritterband DC, Shah MK, et al. Are BAK-free antibiotics susceptible to bacterial contamination?
4918. Bourcier T, Chaumeil C, Borderie V, Laroche L. Antibiotic susceptibility of isolates recovered from bacterial keratitis.
4922. Asbell PA, Epstein SP, Bottone EJ. Susceptibility testing of 100 clinical isolates of Pseudomonas aeruginosa to levofloxacin, moxifloxacin and gatifloxacin.
4924. Shah MK, Miller D, Ritterband D, et al. In-vitro resistant rates for fluoroquinolone antibiotics against methicillin resistant Staphylococcus aureus (MRSA) ocular isolates from different geographic locations.

