 |
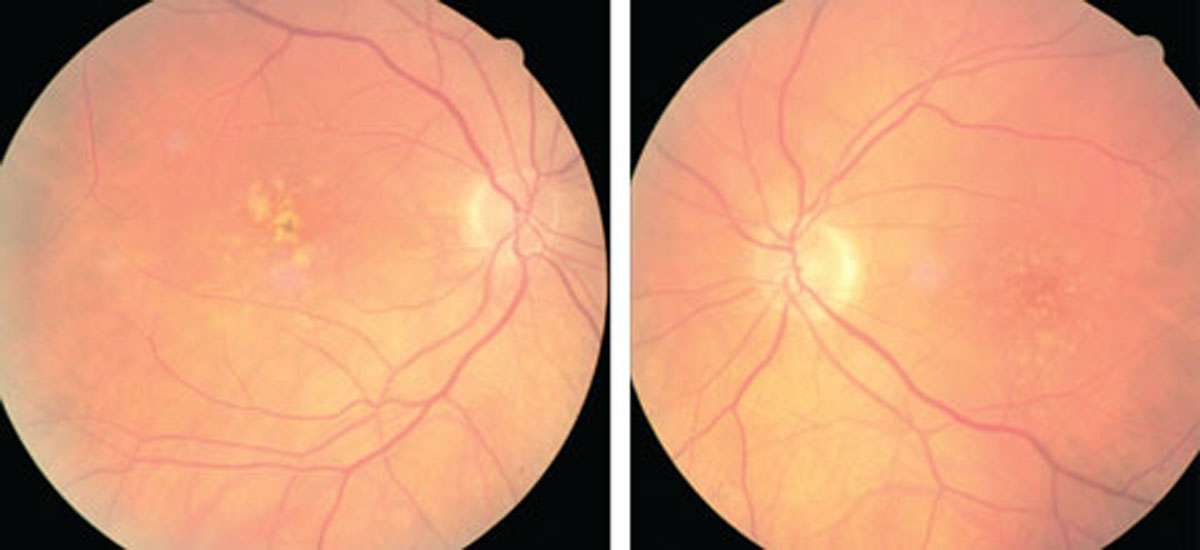
AMD eyes on anti-VEGF are less likely to show a correlation between CST and BCVA. Photo: Julie Poteet, OD. Click image to enlarge. |
Various studies have suggested certain features may be associated with a greater likelihood of specific visual acuity outcomes among groups of eyes receiving treatment for nAMD, but none of these features at baseline nor changes in these features at follow-up have shown a strong correlation with the change in visual acuity for a specific individual. In a recent study, researchers sought to determine the correlation between change in central subfield thickness (CST) and change in best-corrected visual acuity (BCVA) in nAMD eyes receiving anti-VEGF.
Participants were randomized into ranibizumab and aflibercept groups. Weak or no correlation between change in CST and change in BCVA were identified at weeks 12, 52 and 96, which is similar to results from a previous study.
“We believe that the poor correlation between change in CST and change in BCVA in nAMD managed with anti-VEGF therapy may be at least partly due to the influence of other parameters that affect retinal thickness with variable effects on visual outcomes,” the authors explained.
They pointed out that there has been controversy as to whether the treatment regimen may contribute to the strength of the correlation between change in CST and change in BCVA, particularly when change in CST is considered as one of the retreatment criteria in PRN regimens. “In this study at week 52, all eyes had received fixed dosing with an anti-VEGF agent and all correlations were less than -0.1 irrespective of drug or dosing interval. At week 96, all eyes had received the capped-PRN for nearly 12 months and the correlations remained weak at -0.15 in the ranibizumab arm and less than -0.1 in the aflibercept arm,” the authors explained.
Similar results have been reported in nAMD eyes treated with fixed, PRN or treat-and-extend regiments of ranibizumab. “The totality of the evidence suggests that neither agent nor dosing regimen affects the relationship between change in CST and change in BCVA, and that change in thickness is not a good indicator of the functional treatment response,” the authors noted.
They concluded that these findings suggest anatomic differences don’t necessarily correlate with visual acuity differences and that changes in CST should not be used as a surrogate for visual acuity outcomes in nAMD.
Nanegrungsunk O, Gu SZ, Bressler SB, et al. Correlation of change in central subfield thickness and change in visual acuity in neovascular AMD: post hoc analysis of VIEW 1 and 2. Am J Ophthalmol. November 15, 2021. [Epub ahead of print.] |

