A 75-year-old black female presented to ask about having cataract surgery in her right eye. She successfully underwent cataract surgery and IOL implant in her left eye six weeks earlier. Her medical history was significant for hypertension and stomach problems, for which she took Vasotec (enalapril maleate, Merck Frosst) and Prevacid (lansoprazole, TAP Pharmaceutical), respectively.

Best-corrected visual acuity measured 20/30 O.D. and 20/25 O.S. Extraocular motility was full O.U., and cover testing revealed orthophoria. Confrontation fields were full to careful finger counting O.U. Pupils were equally round and reactive with no afferent pupillary defect.
Anterior segment exam in the right eye was significant for 2+ nuclear sclerotic cataract. The left eye had a well-centered posterior chamber IOL with a clear visual axis. IOP measured 19mm Hg O.D. and 17mm Hg O.S.
1,2. Posterior poles in our patient (O.D. left, O.S, right). Despite the hazy view in the right eye from the cataract, note the well demarcated lesion in the macula
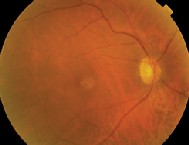

Dilated fundus exam (figures 1 and 2) revealed a moderate-sized cup with good rim coloration and perfusion O.D. A yellow-white, well-circumscribed lesion was present in the macula. We ordered fluorescein angiography (figures 3 and 4) and optical coherence tomography (figure 5).
Dilated fundus exam O.S. revealed an obliquely inserted optic nerve and a generous-sized cup, although this was difficult to determine because of the oblique insertion. The macula, vessels and periphery were normal.
Take the Retina Quiz
1. Which best describes the fluorescein pattern in the right eye?
a. Early hyperfluorescence with late leakage.
b. Early hyperfluorescence with late staining and minimal leakage.
c. Early hyperfluorescence that builds in intensity and fades late.
d. Early hyperfluorescence due to a window defect.
2. What does the OCT show?
a. Pigment epithelial detachment.
b. Neurosensory detachment.
c. Choroidal neovascular membrane (CNVM).
d. Diffuse macular edema.
3. Based on the clinical appearance, fluorescein angiography and OCT, what is the correct diagnosis?
a. Classic CNVM.
b. Fibrovascular pigment epithelial detachment secondary to occult choroidal neovascularization.
c. Serous retinal detachment.
d. Adult vitelliform lesion.
4. What is the etiology?
a. Age-related macular degeneration.
b. Idiopathic.
c. Stress.
d. Nonspecific.
5. What is the correct management?
a. Observation.
b. Laser photocoagulation.
c. Photodynamic therapy.
d. Intravitreal triamcinolone injection.
For answers, click here.
Discussion
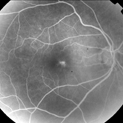
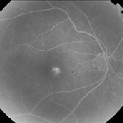
3,4. Early (above) and late shots of the angiogram show hyperfluorescence of the lesion.
The macula of the right eye reveals a well-circumscribed lesion without evidence of subretinal or intraretinal fluid. The cataract makes it difficult to view the lesion and even harder to distinguish some of the more subtle features. Based on the clinical exam, we suspected a choroidal neovascular membrane or an adult vitelliform lesion from a unilateral pattern dystrophy. Fortunately, ancillary testing offered important information to aid our diagnosis.
The fluorescein angiogram showed early hyperfluorescence of the lesion. The hyperfluorescence builds in intensity, and there is minimal late leakage of the dye. Although the staining pattern appears similar to a choroidal neovascularizaiton (CNV), a typical CNV usually results in more late leakage than we see here. This patients staining pattern more likely suggests an occult CNV.
The OCT also suggests occult CNV. The higher reflective area in the macula appears to involve the retinal pigment epithelium. There is no overlying serous detachment, cystoid macular edema or serous pigment epithelial detachment (PED). However, the higher reflective area that we see on OCT represents a fibrovascular PED from an occult CNV.
Two questions remain: What is the etiology, and how do we manage it? Given her age, we might easily assume that her condition is secondary to AMD. However, an absence of drusen in each macula and our patients race suggest otherwise. Her condition is likely idiopathic.
Because her visual acuity is 20/30, we elected to observe her for now. Three months later, the lesion was unchanged, and her acuity remained 20/30. This is very typical of occult CNV. This tends to grow more slowly and often has a smoldering character. By contrast, classic CNV tends to have a more active growth process with leakage and bleeding.
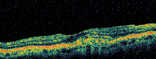
5. OCT of the macular lesion in the right eye shows a highly reflective area.
We will continue to monitor this patient for any change in her acuity or progression of the lesion. If her visual acuity declines, photodynamic therapy would likely be the best treatment because of the subfoveal nature of the lesion.

