Optometrists are no strangers to myopia. In fact, maybe we have become too comfortable with treating this condition, flipping on autopilot mode when prescribing glasses and contacts. It is important to realize that passively “correcting” myopia is simply not enough, especially because we are uniquely positioned and have the tools to proactively prevent, detect and treat it.
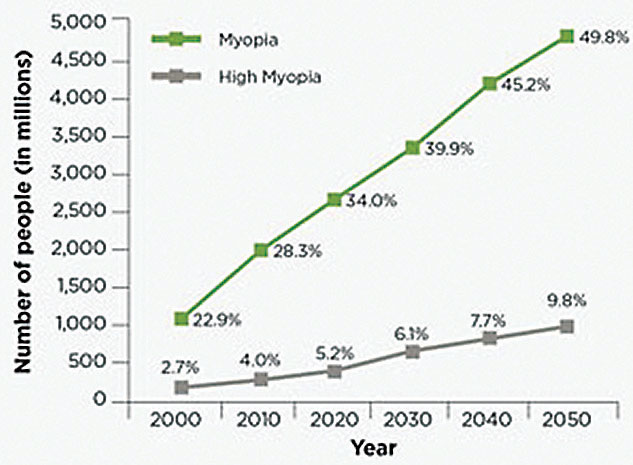
Due to its widespread impact—the global prevalence of myopia has grown by 66% in the past three decades, and it has been estimated that nearly half of the world’s population will be myopic by 2050—myopia has secured a place in the spotlight as a public health issue.1,2 In the United States alone, the prevalence of childhood myopia has increased from 25% to 44% between 1972 and 2004.3,4 As the number of young patients affected by childhood myopia increases, the likelihood of developing high myopia with significant retinal complications later on in life also increases.
With myopia on the rise, we cannot afford to turn a blind eye or do the bare minimum when caring for patients whose lives we have the ability to change. We must emphasize early detection and disease progression control, which should be at the cornerstone of myopia management, and be prepared to treat this population. The following article covers the basics practitioners should consider on their quest to learn more about and manage myopia.
 |
| The global prevalence of myopia has grown by 66% in the past three decades, and it has been estimated that nearly half of the world’s population will be myopic by 2050.1,2 Click to enlarge. |
1. Educate Yourself
‘Why should I practice myopia management?’ is one of the most important questions for practitioners to reflect on. Before attempting to answer it, you must first understand what myopia management means. Identifying and diagnosing myopia is generally easy and straightforward. Knowing how to prevent myopia from progressing, however, proves to be harder; it involves clinical expertise and patient compliance.
As you delve into the core of myopia management, be prepared to step out of the ‘phoropter zone’ and start thinking beyond the fovea. Numerous animal studies have shown that the peripheral retina—not the fovea—plays an integral part in axial length (AL) growth.5-7 With that being said, this finding does not come without controversies. Currently, a foolproof theory or formula that can completely ‘control’ myopia does not exist. It is worth noting that, at the moment, there are no FDA-approved treatments for myopia management. Practitioners should be forthright when discussing this with patients and their parents. Rather than making absolute claims and asserting that treatment will prevent myopia from worsening, which is impossible anyway, practitioners must manage myopia based on each patient’s myopia profile to render more promising prognoses and treatment outcomes.
When managing myopia, it is important that practitioners set a clear goal and have a focused mindset to develop treatment plans for young patients best suited under the circumstances. Currently, there are three evidence-based approaches that are commonly used for myopia management—orthokeratology (ortho-k), soft multifocal contact lenses and topical compounded atropine. Each modality offers unique benefits and challenges.
Ortho-k is generally geared toward young, athletic patients who show little to no contraindications or corneal irregularities, such as keratoconus. Capturing good quality baseline corneal topography is vital.
Soft multifocal contact lenses with custom designs are typically catered toward patients with high myopia and atypical astigmatism, for which ortho-k may not be able to provide satisfactory uncorrected vision during the day, or those who do not adapt well to rigid gas permeable lenses at night.
Topical compounded atropine is generally used for young patients who manifest atypical, rapid myopia progression and a strong inheritance of myopia and are not compliant with contact lens wear. Aside from the technical expertise necessary to fit contact lenses, myopia management is unique in that it combines technical and behavioral approaches to address the distinct myopia profile of each patient.
While dabbling in myopia management helps you get your feet wet, unfortunately it does not get you very far. Specializing in myopia management requires practitioners devote significant amounts of time and effort, refine other areas of their practices to move myopia management to the forefront and allocate staff and resources.
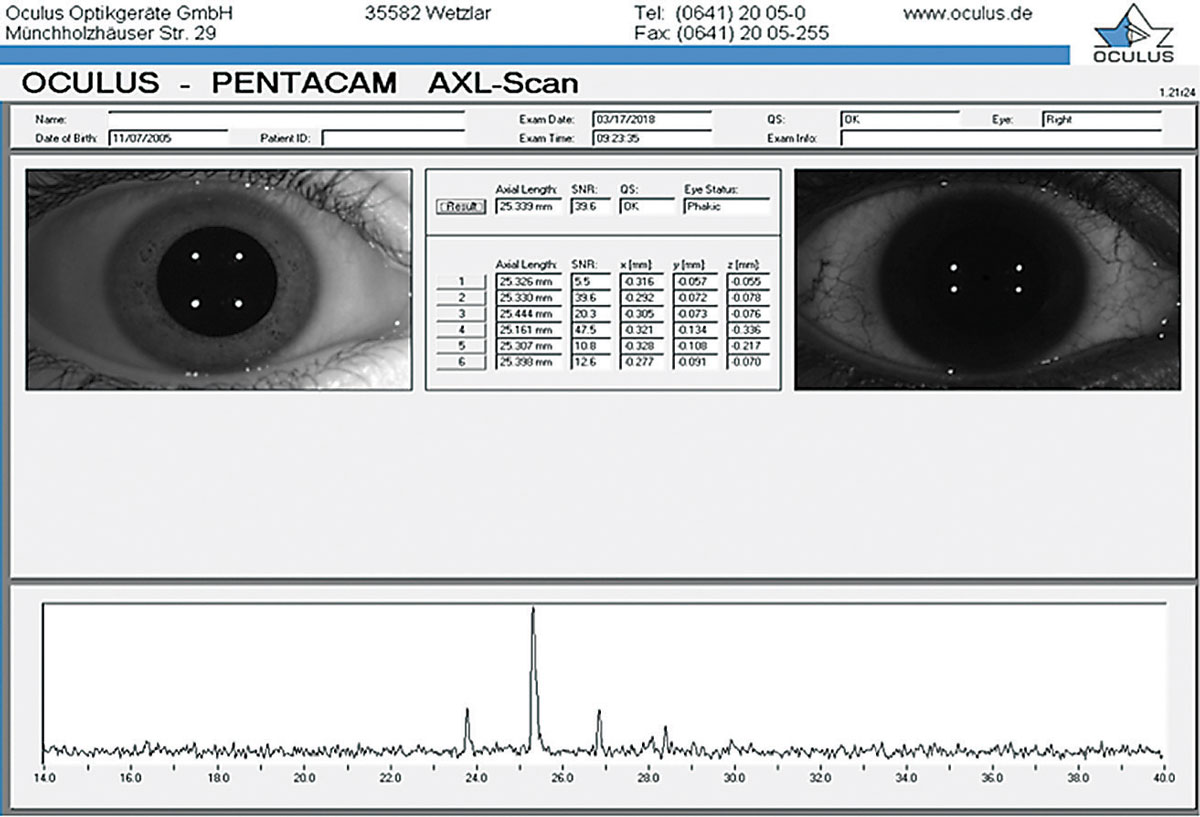 |
| The Pentacam Scheimpflug imaging system is an important tool used to analyze the anterior segment and measure AL to help guide myopia management. |
2. Stock Your Practice
The process begins with acquiring the resources necessary to manage myopia, starting with tools and technologies. Managing myopia involves using more just a phoropter. Having a corneal topographer is fundamental and helps practitioners understand patients’ corneal health and determine which management strategy is best suited under the circumstances. For example, using corneal topography to learn more about a patient’s corneal elevation differentials, such as the relationship between sagittal height differentials (SHDs) and corneal toricity, would help guide lens design if corneal reshaping or ortho-k were being considered as treatment modalities. A recent study showed that a higher corneal toricity is more likely to result in lens decentration.8,9 As a result, custom lens parameters are designed to optimize lens centration. Additional studies have found that toric ortho-k lenses are preferred to minimize lens decentration when SHDs exceed 30µm at a chord length of 8mm.9,10
Measuring AL has become the foundation of myopia management. Many sophisticated technologies—such as the IOLMaster (Zeiss), one of the most popular instruments for obtaining AL measurements—are now able to detect microscopic physiologic variations that often precede subjective dioptric changes manifested by phoropters. Currently, the sonographic A-scan and the non-contact automatic Pentacam corneal tomographer are among the more commonly used pieces of equipment. Both have their advantages and shortcomings. The A-scan is generally light and portable, making it easier to transport between offices, and more affordable. However, operating the A-scan requires direct tactile contact using an ultrasound probe on the cornea under topical anesthesia, steady fixation and proper posture. Using this device while working with children may prove to be difficult; putting a probe onto their eyes can be intimidating and technically challenging.
The Pentacam, on the other hand, uses a high-resolution rotating Scheimpflug imaging system to capture panoramic views of the cornea and provide a precise anterior segment analysis and elevation maps of the anterior and posterior corneal surface and thickness. The newest version of the Pentacam incorporates AL measurement technology, is precise and does not involve tactile contact with the cornea or topical anesthesia. All in all, it is generally more practical and favorable when working with children.
 |
This child is undergoing Pentacam Scheimpflug imaging. |
3. Prepare Staff
As you are building your myopia management armamentarium, you should be allocating and educating your staff and determining an action plan. It is worth delegating tasks and designating a few technicians and staff members to a ‘core staff team’ that has more in-depth education and training and can take on more responsibilities to alleviate the burden on you and enhance the patient experience.
Patient consultations may take an hour to obtain in-depth information to construct effective treatment plans but vary on a case-by-case basis and should not be rushed or associated with a time restraint. To make matters easier, myopia patients should be scheduled on the same day.
In my experience with post-treatment care for myopia management, patients who receive the overnight ortho-k modality are generally seen for monitoring a day after, a week after and a month after treatment, at which point they are seen on a quarterly basis for the remainder of the first year of treatment. Once stable, I follow up with patients on a quarterly or biannual basis depending on the situation. If treated with topical compounded atropine, patients are typically monitored for near vision quality and photophobia issues in quarterly intervals.
Unlike adults, young patients may not always be able to comfortably or effectively express their experience clearly and accurately. Be on the lookout for clues of discomfort or dissatisfaction, which are usually reflected via nonverbal cues and body language. A recent cognitive study found that nonverbal, communicative eye contact yields anticipatory cooperation and commitment in children.11 This patient population requires more than your typical ‘five-minute-check-and-go’ follow-up and may greatly benefit from additional face-to-face time with you, the practitioner, to establish a sense of familiarity, comfort and rapport. Practitioners and staff alike need to be prepared to exercise patience and work with this unpredictable demographic—perhaps by implementing an incentive or reward program—otherwise, young patients may feel neglected or misunderstood, which may result in compliance issues and negative visual outcomes.
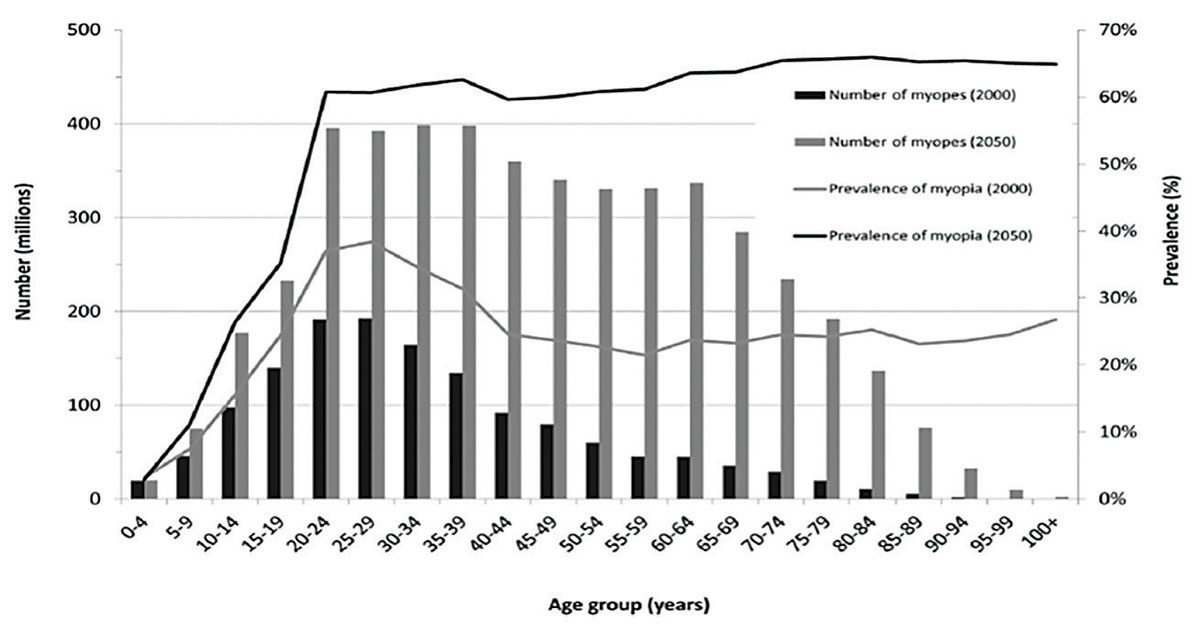
| The Future is Looking Myopic By Catherine Manthorp, Associate Editor Myopia was previously thought to be a simple refractive condition correctable by glasses and contact lenses with limited visual consequences. We know now this is simply not the case; the condition is increasingly associated with a heightened risk of permanent vision impairment.1 A groundbreaking 2016 study by the Brien Holden Vision Institute on the global prevalence of myopia and high myopia since 1995 found that myopia affected 23% of the world’s population, or 1.5 billion people, in 2000.2 Using the data they obtained to predict what the future prevalence of myopia looks like, the team cautioned that half of the global population—that’s five billion people—could be affected by 2050.2 To make matters worse, while only 3%, or 163 million people, had high myopia in 2000, this percentage is expected to increase to 10% by 2050.2 That means one billion people could be at risk of permanent vision impairment and blindness, which would make myopia the leading cause of blindness worldwide.2 Luckily, the researchers narrow in on the problem by shedding light on what is causing this shift, which demographic is experiencing the greatest impact and what can be done about it. Environmental influences and lifestyle changes—such as reduced time outdoors, increased near activities, higher-pressure educational systems and greater electronic device usage—are two of the biggest factors at play.3 In 2000, myopia was occurring for the most part in patients younger than 40, indicating that these factors mainly affected this demographic.2
If practitioners don’t assert control, myopia’s inexorable growth could eventually leave most patients either affected directly or at least indirectly feeling its consequences through the effects on a family member. 1. Jong M, Sankaridurg P, Fricke TR, et al. Myopia on the move. RCCL. 2017;154(1):12-5. 2. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42. 3. Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379:1739-48. |
4. Initiate Patient Acquisition Marketing Efforts
As you equip your practice with educated staff members and appropriate tools, you should begin mapping out and executing your marketing plan. As with raising awareness about anything, digital marketing is a great way to introduce the myopia management services your practice is offering. According to recent statistics, approximately 74% of Internet users actively engage in social media, 80% of who specifically search for medical information and resources.12 Nevertheless, only 26% of medical professionals in large corporations or hospitals in the United States use social media as a tool to market their medical services.12 Clearly, consumers have an appetite for social media, giving us a great opportunity to give them a platform catered toward myopia management.
The success of any marketing campaign depends on how well the audience is targeted. Because myopia management services are primarily geared toward children, it is the baby boomers and the Gen X’ers—the parents (decision-makers) of most of today’s myopic kids—that we need to reach. Volunteering to speak at local community events and provide vision screening in schools and pediatricians’ offices are good ways to increase public awareness of early preventative eye care and your unique service for children.
Perhaps most importantly, and free of cost to you, you should consider focusing your efforts within your own practice through internal marketing. You will probably find that your patients, many of whom may be young myopes, are your best source of marketing. Raising awareness of the additional services you offer through discussions or handouts leads to word-of-mouth referrals and increases traffic flow to greatly benefit your practice. You can also look toward your colleagues who have myopic children because treating local physicians’ kids for myopia management allows you to provide a first-hand experience of your services to medical professionals who can vouch for you when making referrals.
5. Consult and Counsel
“If you’re a refraction-centric optometrist, you’re going to be replaced by technology,” predicts Dr. Thomas. “But if you’re a medically oriented optometrist, there’s nothing out there to replace solid cerebral clinical judgment.” This is a common sentiment among optometrists and it’s driven many changes in both legislation and education, both of which are facilitated by technological advances that are making it possible for ophthalmologists and optometrists alike to function more precisely, with more robust data and, ultimately, practice at higher levels.
After acquiring patients, but before starting myopia management, comes the consultation stage. A thorough myopia consultation typically involves obtaining a detailed case history, which includes gender, ethnicity, age at myopia diagnosis, age at myopia correction, average rate of myopia progression, ocular history and congenital medical conditions. It is also worth taking the time to understand your patient’s lifestyle to help facilitate patient education and guide the treatment process.
Based on a patient’s history and lifestyle, practitioners can determine who is at risk of myopia progression. Ethnicity plays a large and independent role in the development and progression of myopia. In particular, children of Asian and Southeastern descent are inheritably at a higher risk of early onset of myopia.13,14 Moreover, several studies have shown that increasing the amount of near work activities, especially on digital devices, and reducing the amount of time spent outdoors are associated with increased odds of myopia development.15-22
Consultation does not end after learning about your patient’s background. Many parents are not properly educated about myopia in terms of its risk factors, signs and increasing prevalence and the implications of higher degrees of myopia. While parents acknowledge their children have vision problems, they have yet to associate worsening vision with greater risks of retinal and other eye health complications and understand how to address these issues. As a result, proper and timely intervention for childhood myopia may not occur.
An observational study reported that 55% of participants had never taken notes during a medical appointment, and 41% were reluctant to disclose their medical concerns to their physicians because they felt rushed during their consultation.23 Therefore, it is crucial to allow 20 to 30 minutes for parents to engage in Q&A sessions and discuss realistic goals and expectations. It is also vital that clinicians carefully delineate the relationship between refractive changes and eye health consequences to help patients and their parents better understand and appreciate the long-term ocular health benefits of myopia management.
6. Discuss the Finances
It is important to discuss the costs of this condition, which may not be on most parents’ radar, with already anxious parents who may be trying to decide how they are going to pay for your services or if they are even worth it in the first place.
“Is this covered by insurance?” is one of the questions parents most frequently ask. Currently, myopia management is generally uncovered and is ‘elective.’ It is also not ‘medically necessary’ as per the current standard of care. Criteria that qualify as ‘medically necessary’ include corneal irregularities (e.g., keratoconus and post-surgical corneal complications), high myopia (-10D) and hyperopia (+10D) and aphakia.24 Contact lenses are usually covered when vision correction by custom lenses yields far superior visual outcomes than conventional spectacles. While conventional contact lenses may be covered by most vision plans, lenses for myopia management are not.
There are, however, other options. flex spending accounts and health spending accounts are generally accepted. Third-party healthcare finance companies can be used as well. Regardless of insurance coverage, it is critical to have candid discussions with parents regarding their financial situations without overwhelming them. Should they decline to proceed with myopia management, parents must be aware of the cumulative costs of conventional spectacles or contact lenses both financially and medically.
You cannot afford to take any shortcuts when developing a first-class myopia management practice and making it your own. Given the growing prevalence of myopia, you must be prepared to work with patients who are interested in enlisting your services and offer them the best care possible through the resources, effort and time you allot. While it has its challenges, managing myopia is also extremely rewarding, sets your practice apart from others and allows you to use your passion and expertise to change the lives and vision of your patients.
Dr. Chan is the director of Treehouse Eyes in Tysons Corner, VA, and a fellow of the American Academy of Optometry. He graduated with a doctorate in optometry and a masters in vision sciences from the New England College of Optometry.
| Myopia Education Efforts Online and Abroad By Mark De Leon, Associate Editor Myopia may be pervasive, but so are efforts to spread awareness and inform ways to reduce progression. Resources abound. Essilor has taken big steps in furthering the conversation about myopia on a global scale, with a longstanding commitment to education and intervention, including assistance in launching the first National Myopia Management Convention in Singapore last June.1 Stateside, Essilor spread myopia awareness last fall with a movie trailer that screened in select theaters nationwide, to inspire parents to be vigilant for warning signs in their children and schedule a comprehensive eye exam.2 Clinicians can also download a variety of educational tools at essilorshare.com/myopia. Early this month, the company announced the formation of a Myopia Taskforce comprised of 14 experts “who have pledged their commitment to establishing a preferred method for comprehensive myopia care, including developing a universally accepted care protocol for managing myopia,” according to Vision Monday.3 It’s part of Essilor’s Myopia Initiative in Action, which will be rolling out this year. In November, Johnson & Johnson Vision teamed up with experts, also in Singapore, on a research collaboration to tackle myopia.4 The aim is to create tools to identify those at risk to develop high myopia, learn about the underlying mechanisms of myopia and work toward developing better treatments. The Brien Holden Vision Institute (BHVI) recently launched its online Global Myopia Centre, which includes numerous free online tools, such as BHVI’s Myopia Calculator, Guidelines for Myopia Management and online courses that provide accredited training for practitioners in myopia interventions.5 You can access them here: www.globalmyopiacentre.org. At the 2018 Academy of Optometry meeting, the International Myopia Institute presented seven white papers on areas such as myopia definitions, evidence for interventions, ethical considerations, clinical trial guidelines and clinical management guidelines.6 The reports will be available at the beginning of this year in Investigative Ophthalmology and Visual Science. Kate Gifford, PhD, chair of the institute’s clinical management committee, has been managing myopia for over 15 years. With her husband, Paul Gifford, PhD, she developed various patient communication resources, including the Myopia Profile tool, available at myopiaprofile.com. Dr. Gifford uses the profile tool whenever she examines a child who is already myopic or shows risk of developing the condition. The duo has also developed My Kid’s Vision (www.mykidsvision.org) as another information resource to help parents understand myopia and the steps they can take toward prevention and the slowing of progression.
Visioneering Technologies, which makes the NaturalVue contact lens for myopia control, supported the development of www.managemyopia.org, a website for practitioners looking to better address the needs of myopic patients, which includes screening tools and other resources. CooperVision offers the MiSight contact lens for myopia control outside the US and is studying it in ongoing trials. The company provides an educational summary for the public with advice on how parents can keep myopia at bay (coopervision.com/blog/three-ways-to-slow-down-myopia) and advice for clinicians as well (coopervision.com/practitioner/clinical-resources/myopia-control-in-youth). Industry has also been raising awareness of the link between digital screen use and myopia, as well as dry eye. In June, Shire launched Screen Responsibly (www.myeyelove.com/screen-responsibly), a consumer-friendly resource to ensure a healthy screen routine. It doesn’t always take an entire industry to generate discourse among an engaged community of optometrists. It just takes commitment and conversation. Each OD can make meaningful differences in patients’ lives with a little more attention and emphasis for those at risk. 1. Leading the fight against myopia, starting in Singapore [news release]. Essilor; June 22, 2018. www.essilor.com/en/medias/news/leading-fight-myopia-starting-singapore/. Accessed December 19, 2018. 2. As myopia rates rise in the U.S., Essilor of America launches initiative to help combat growing vision issue [press release]. Dallas: PR Newswire; September 20, 2018. www.prnewswire.com/news-releases/as-myopia-rates-rise-in-the-us-essilor-of-america-launches-initiative-to-help-combat-growing-vision-issue-300716218.html. Accessed December 19, 2018. 3. Essilor of America Forms Taskforce to Combat Growing Myopia Epidemic in U.S. www.visionmonday.com/latest-news/article/essilor-of-america-forms-taskforce-to-combat-growing-myopia-epidemic-in-us 4. Singapore National Eye Centre, Singapore Eye Research Institute and Johnson & Johnson Vision set sights on halting global Myopia epidemic [press release]. Singapore: Johnson & Johnson Vision; November 12, 2018. www.jjvision.com/press-release/singapore-national-eye-centre-singapore-eye-research-institute-and-johnson-johnson. Accessed December 19, 2018. 5. Brien Holden ‘Global Myopia Centre’ a new ‘one-stop’ resource platform [news release]. San Antonio, TX: Brien Holden Vision Institute; November 7, 2018. www.brienholdenvision.org/news/item/176-brien-holden-global-myopia-centre-a-new-one-stop-resource-platform.html. Accessed December 19, 2018. 6. Carter H. Clinical guidelines for myopia in white paper. Optometry Australia. November 23, 2018. www.optometry.org.au/blog-news/2018/11/23/clinical-guidelines-for-myopia-in-white-paper/. Accessed December 19, 2018. |
1. Fricke TR, Jong M, Naidoo KS, et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modeling. Br J Ophthalmol. 2018;102(7):855-62. 2. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42. 3. Kempen JH, Mitchell P, Lee KE, et al. The prevalence of refractive errors among adults in the United States, Western Europe and Australia. Arch Ophthalmol. 2004;122(4):495-505. 4. Vitale S, Sperduto RD, Ferris FL 3rd. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127(12):1632-9. 5. Bowrey HE, Zeng G, Tse DY, et al. The effect of spectacle lenses containing peripheral defocus on refractive error and horizontal eye shape in the guinea pig. Invest Ophthalmol Vis Sci. 2017;58(5):2705-14. 6. Schaeffel F, Feldkaemper M. Animal models in myopia research. Clin Exp Optom. 2015;98(6):507-17. 7. Tse DY, Lam CS, Guggenheim JA, et al. Simultaneous defocus integration during refractive development. Invest Ophthalmol Vis Sci. 2008;48(12):5352-9. 8. Maseedupally VK, Gifford P, Lum E, et al. Treatment zone decentration during orthokeratology on eyes with corneal toricity. Optom Vis Sci. 2016;93(9):1101-11. 9. Li Z, Cui D, Long W, et al. Predictive role of paracentral corneal toricity using elevation data for treatment zone decentration during orthokeratology. Curr Eye Research. 2018;43(9):1083-9. 10. Chen Z, Feng X, Jiaqi Z, et al. Prediction of orthokeratology lens decentration with corneal elevation. Optom Vis Sci. 2017;94(9):903-7. 11. Siposova B, Tomasello M, Carpenter M, et al. Communicative eye contact signals a commitment to cooperate for young children. Cognition. 2018;179:192-201. 12. Social media and health care by the numbers. Southern Medical Association. sma.org/social-media-healthcare-by-the-numbers/. Published July 12, 2017. Accessed December 3, 2018. 13. Pan C, Ramamurthy D, Saw S. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2011;32(1):3-16. 14. Theophanous C, Modjtahedi BS, Batech M, et al. Myopia prevalence and risk factors in children. Clin Ophthalmol. 2018;12:1581-7. 15. Ashton GC. Nearwork, school achievement and myopia. J Biosoc Sci. 1985;17(2):223-33. 16. Huang H, Chang DS, Wu P, et al. The association between near work activities and myopia in children—a systematic review and meta-analysis. Plos One. 2015;10(10). 17. Ku P, Steptoe A, Lai Y, et al. The associations between near visual activity and incident myopia in children. Ophthalmology. June 19, 2018. [Epub ahead of print]. 18. Li S, Li S, Kang MT, et al. Near work related parameters and myopia in Chinese children: the Anyang Childhood Eye Study. Plos One. 2015;10(8). 19. Rose KA, Morgan IG, Smith W, et al. Myopia, lifestyle and schooling in students of Chinese ethnicity in Singapore and Sydney. Arch Ophthalmol. 2008;126(4):527-30. 20. Walline JJ, Smith MJ. Controlling myopia progression in children and adolescents. Adolesc Health Med Ther. 2015;6:133-40. 21. Wu P, Chen C, Lin K, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. 2018;125(8):1239-50. 22. Xiong S, Padmaja S, Thomas N, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmologica. 2017;95(6):551-66. 23. Carman KL, Maurer M, Yegian JM, et al. Evidence that consumers are skeptical about evidence-based health care. Health Affairs. 2010;29(7):1400-6. 24. Davis RL. Medically necessary contact lenses: medical plan or vision plan responsibility? RCCL. 2016;153(5):36-9. |