 A 10-year-old
Hispanic male presented to the emergency room with his parents immediately following
a BB gun injury to his left eye. The boy’s eye was significantly red, and he
reported moderate pain and very blurry vision.
His best-corrected visual acuity measured 20/20 O.D. and
20/80 O.S. Confrontation visual fields were full to careful finger counting
O.U. His pupils were both equally round and reactive, with no afferent
pupillary defect.
A 10-year-old
Hispanic male presented to the emergency room with his parents immediately following
a BB gun injury to his left eye. The boy’s eye was significantly red, and he
reported moderate pain and very blurry vision.
His best-corrected visual acuity measured 20/20 O.D. and
20/80 O.S. Confrontation visual fields were full to careful finger counting
O.U. His pupils were both equally round and reactive, with no afferent
pupillary defect.
The anterior segment examination of his right eye was normal; however, his left eye showed significant lid swelling and a lower lid laceration. Additionally, he had a significant subconjunctival hemorrhage nasally and inferiorly. His left cornea was clear, and the anterior chamber was 3+ deep, but we noted a minimal hyphema. The iris was flat, the pupil was round and there was no iris dialysis present in his left eye. The lens was also clear. His intraocular pressure measured 17mm Hg O.U. Dilated fundus exam of the right eye was completely normal. The left optic nerve had a small cup with good rim coloration and perfusion. Additionally, the patient had a diffuse vitreous hemorrhage in his left eye.
 |
 |
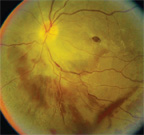
| 1. A fundus montage of the posterior pole and peripheral
retina of our patient’s left eye two days after being shot with a BB.
|
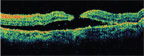
2. The OCT through the macula shows a shallow serous detachment two days after the injury. |
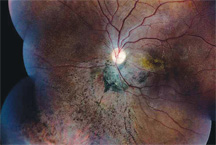
We saw the patient two days later. His hyphema had cleared, and his feelings of pain and discomfort had improved. But, his visual acuity had dropped to 20/200 O.S. We took fundus photographs (figure 1) and performed an optical coherence tomography scan (figure 2). We saw the patient one week later, and his visual acuity had diminished to 20/400 O.S. Again, we took fundus photographs (figure 3) and performed an OCT scan (figure 4).
 |
 |
| 3. A posterior pole image of our patient one week after the
injury.
|
4. A second OCT through the macula one week after the injury. What specific finding does it confirm? |
Take the Retina Quiz
1. What does the extensive retinal whitening in the posterior pole and peripheral retina of the patient’s left eye represent?
a. Retinal detachment.
b. Choroidal rupture.
c. Berlin’s edema.
d. Commotio retinae.
2. What does the lighter-colored area in the far periphery of his left eye likely represent?
a. Open globe, perforating injury.
b. Sclopetaria.
c. Choroidal rupture.
d. Chorioretinal atrophy.
3. What further testing would be helpful in the management of this patient?
a. CT scan.
b. Visual field.
c. Ultrasound.
d. Both a and c.
4. What do the one-week follow-up examination and OCT of the patient’s left eye reveal?
a. Chorioretinal scarring.
b. Retinal detachment.
c. Full-thickness macular hole.
d. Pseudohole.
5. How should this patient be managed?
a. Observation.
b. Repair of the retinal detachment.
c. Repair of the full-thickness macular hole.
d. Laser procedure.
For answers, see below.
Discussion
The retinal whitening seen throughout the posterior pole and retina of our patient’s left eye represented large areas of commotio retinae. He also exhibited a vitreous hemorrhage that obscured some of the peripheral retinal detail; however, there was a circular white area in the far periphery that may have represented either sclopetaria or a choroidal rupture. It is worth noting that this case was similar to another that I discussed in 2007, in which a 12-year-old boy presented with a traumatic macular hole and retinal sclopetaria following a BB gun injury to his left eye (“Small BB, Big Problems,” June 2007). Because of the vitreous hemorrhage, the ER ophthalmologist who initially saw the patient could not completely rule out the presence of a retinal detachment––so, he scheduled an ultrasound. The ultrasound revealed no retinal detachment. OCT was also performed at this time, which revealed the presence of serous fluid underneath the macula.
| ‘You’ll Shoot Your Eye Out’
Nearly 30,000 Americans present to ERs with BB- and pellet gun-related injuries each year.2,3 Most incidents are unintentional and typically occur in young males. One surveillance report of approximately 47,000 BB gun-related injuries conducted by the Centers for Disease Control and Prevention between June 1992 and May 1994 suggested that more than 50% of injuries occurred in children between 10 and 14 years of age, and that 2,839 (6%) of patients suffered direct eye trauma.1 |
The patient was seen a week later and reported feeling much better; however, he believed his vision had become worse in his left eye. Indeed, on clinical examination it appeared that the patient developed a full-thickness macular hole, which was confirmed on OCT. Additionally, the patient still had a considerable vitreous hemorrhage. Still, we were able to see sufficient detail of the peripheral retina to rule out a retinal detachment. Because the patient developed a full-thickness macular hole, we scheduled him for a pars plana vitrectomy and a membrane peel. At the conclusion of the surgery, long-acting gas was injected into the patient’s vitreous and he was instructed to remain facedown for one week.
We instructed the patient to return one week after the surgery, and then again in one month. At the one-month follow-up, his vision measured 20/200 O.S. and the hole appeared closed on careful fundus examination. We confirmed this finding on OCT. Considering the amount of damage that our patient’s eye sustained, his outcome was exceptional. Most remarkable, however, was that his macula demonstrated complete closure of the full-thickness hole, resulting in an excellent visual outcome. He suffered extensive commotio retinae, which was seen throughout the posterior pole, extending inferiorly. This appeared as an area of retinal whitening and a loss of retinal transparency due to disruption and swelling of the photoreceptor outer segments as a direct result of the BB impact. Interestingly, the retinal whitening almost completely resolved within one week of the injury.
 |
| 5. A fundus montage 10 weeks after the injury. What do you see? |
Because of the retinal damage, not only did the photoreceptors degenerate, but also pigment from the retinal pigment epithelium (RPE) migrated forward into the sensory retina. Clinically, this was seen at six weeks following the injury and was captured on funduscopy at 10 weeks. The fundus images revealed extensive RPE hyperplasia and bone spicule pigmentation located inferiorly within the sensory retina (figure 5). At the initial exam, we believed that our patient had an area of sclopetaria, which represents a full-thickness break that affects the retina, RPE and choroid. It results from a closed-globe injury when a missile-like object tangentially bumps, but does not penetrate, the eye wall. The contusion injury causes a rupture of the choroid, Bruch’s membrane and retina, yet leaves the sclera intact.1 Typically, severe scarring develops around the area where the rupture occurred. It was difficult to determine whether our patient had sclopetaria (like the boy in 2007) or a choroidal rupture. Typically, the BB would have had to penetrate the lid and hit the outer globe tangentially in a missile-like fashion to cause sclopetaria. Though it is possible that the trauma occurred in this fashion, the CT scan revealed no external foreign body.
At his most recent exam, our patient’s visual acuity measured 20/60 O.S. His IOP was normal, despite the presence of a large-area angle recession. Also, he exhibited very minimal subluxation of the crystalline lens, which was seen only upon dilation. We will continue to monitor him closely.
1. Annest JL, Mercy JA, Gibson DR, Ryan GW. National estimates of nonfatal firearm-related injuries. Beyond the tip of the iceberg. JAMA. 1995 Jun 14;273(22):1749-54
2. McNeill AM, Annest JL. The ongoing hazard of BB- and pellet gun-related injuries in the United States. Ann Emerg Med. 1995 Aug;26(2):187-94.
3. The U.S. Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report: BB- and Pellet Gun-Related Injuries––U.S., June 1992-May 1994. Available at: www.cdc.gov/mmwr/preview/mmwrhtml/00039773.htm (Accessed September 20, 2009).
Answers to the Retina Quiz: 1) d; 2) b; 3) d; 4) c; 5) c.

