 |
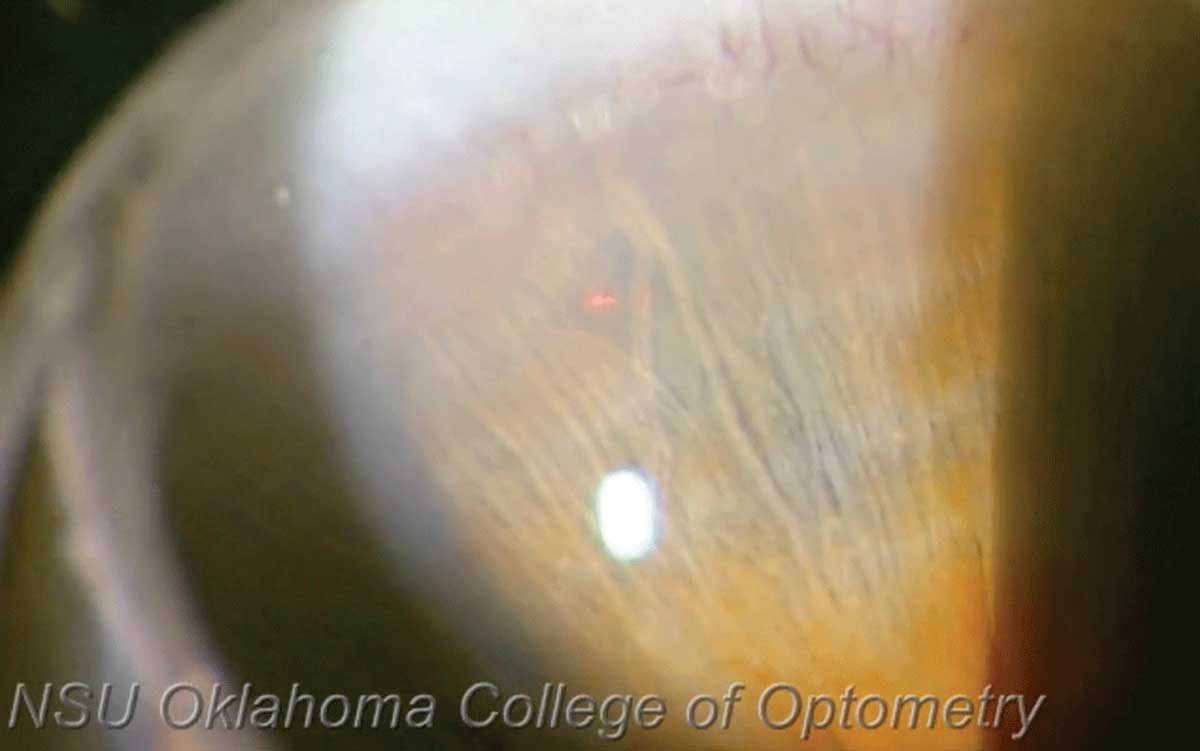
| Black patients in this study were shown to be more prone to increased IOP after LPI. Photo: Joseph Shetler O,D, and Nathan Lighthizer, OD. Click image to enlarge. |
While laser peripheral iridotomy to reduce the risk of primary angle-closure glaucoma is routine for many eye care providers, the factors that determine short-term complications post-procedure are not fully understood. To address this gap, researchers sought to evaluate the impact of patient characteristics and laser type on IOP elevation and iritis incidence.
In this single-center retrospective study, a team reviewed the electronic medical records of 1,485 primary angle-closure suspects (2,407 eyes) who underwent either Nd:YAG or sequential argon and Nd:YAG laser peripheral iridotomy. Of the included patients, 70.4% were female, 43.4% were Black and 45.6% were non-Hispanic white.
Data collected included average IOP within 30 days prior to laser peripheral iridotomy, post-laser peripheral iridotomy IOP within one hour, laser type, laser energy and the incidence of new iritis within 30 days of the procedure.
The researchers reported that the incidence of post-procedure IOP elevation and iritis was 9.3% and 2.6%, respectively. Multivariate analysis revealed that self-identified Black patients had significantly higher rates of post-laser peripheral iridotomy IOP elevation compared with their white counterparts (13.3% vs. 5.5%). This was also the case for post-procedure iritis, with a rate of 4.4% observed in Black patients vs. 1.1% among white individuals.
Additionally, the data showed that Asian race is not significantly associated with immediate post-laser peripheral iridotomy IOP elevation or iritis. This suggests, according to the investigators, that there are other clinically significant risk factors for both conditions aside from iris thickness and pigmentation.
The findings also demonstrated that higher baseline IOP was associated with an increased risk for post-laser peripheral iridotomy IOP elevation; however, laser type and energy were not correlated with either post-procedure IOP elevation or iritis.
“Results suggest Black patients and those with higher pre-procedure IOP would benefit from additional medications to mitigate the effects of immediate IOP elevation and decrease the incidence of iritis,” the study authors concluded. “Further investigation with a prospective trial is necessary to not only verify these results, but also to yield insight into the optimal management, duration and long-term sequelae of post-laser peripheral iridotomy IOP elevation and iritis in Black patients.”
Adetunji MO, Meer E, Whitehead G, et al. Self-identified black race is a risk factor for intraocular pressure elevation and iritis following prophylactic laser peripheral iridotomy. J Glaucoma. February 4, 2022. [Epub ahead of print]. |

