 |
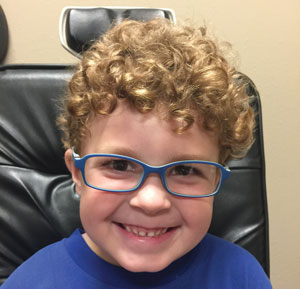
| Glasses remain the mainstay option for most cases of amblyopia but newer, computer-based options may allow kids to skip this method. Photo: Erin Jenewein, OD. |
Digital therapeutics are becoming increasingly common in the management and treatment of various diseases and conditions such as ADHD, asthma, insomnia and substance abuse disorder. Now, software-based intervention is even being used for patients with amblyopia, the number one cause of visual impairment in childhood, affecting around 3% of children. Dichoptic therapy is an approach that aims to rebalance visual stimuli between the eyes, thereby reducing suppressive interactions in the visual cortex. To make this treatment accessible to patients at home, researchers developed and conducted a trial using Luminopia One, a technology designed to deliver dichoptic amblyopia therapy through an interactive patient experience. Note: the manufacturer funded this study.
A total of 105 children with amblyopia, aged five to seven, enrolled in 21 participating clinical sites around the United States to participate in the 12-week study. Each patient had either a diagnosis of unilateral amblyopia associated with strabismus, anisometropia or both combined. They were divided into two groups: the treatment group, in which patients used the therapeutic at-home for one hour/day, six days/week plus full-time glasses; and the comparison group, in which patients continued full-time glasses with no other treatment. Best-corrected VA measurements were captured using logMAR values and changes in VA are reported as lines (change of 0.10 logMAR = one line).
Children in the treatment group could choose what to watch from a library of TV shows and movies, which were then modified by the software in real-time into therapeutic visual stimuli, streamed using WiFi and delivered dichoptically to the patient within a head-mounted display. The two therapeutic modifications were as follows: (1) the total contrast of images shown to the fellow eye was reduced to 15% of that shown to the amblyopic eye and (2) complementary dichoptic masks were superimposed on the images so that children needed both eyes to fully appreciate the video content.
By the end of the 12 weeks, the amblyopic eye VA showed a greater improvement of 1.8 lines (0.18 logMAR) in the treatment group compared with 0.8 lines (0.08 logMAR) in the continued glasses group. In addition, 62% of patients in the treatment group experienced a VA improvement in the amblyopic eye of ≥two lines from baseline, while only 33% in the continued glasses group were able to achieve this. No serious adverse effects were observed in either group.
“The time course of primary outcome data between groups suggests that amblyopic eye vision may have reached a plateau in the continued glasses group by eight weeks while continuing to improve in the treatment group through the 12-week primary outcome,” the researchers explained in their paper. “Future studies should investigate the value of extending treatment duration for maximum benefit from the therapeutic.”
Patients also maintained compliance and reported high levels of satisfaction throughout the study, which researchers attribute to the personalization of the treatment that allowed children to choose which content they consumed from their own homes.
“Our results support the hypothesis that patient satisfaction with digital therapeutics may encourage adherence in at-home settings,” the researchers conclude.
Xiao S, Angjeli E, Wu HC, et al. Randomized controlled trial of a dichoptic digital therapeutic for amblyopia. Ophthalmology. September 13, 2021. [Epub ahead of print]. |

