Ocular Surface HealthCheck out the other feature articles in this month's issue:- Lid Wiper Epitheliopathy: What the OD needs to know - Red Eye Remedies: New and Tried-and-True - How to Answer the "Why?" of Dry Eye - A Modern Approach to Meibomian Gland Dysfunction (earn 2 CE credits) |
Tear supplementation with artificial tears is traditionally considered a first-line treatment for dry eye disease (DED). While these agents don’t target the underlying pathophysiology, they often help to alleviate symptoms.1
Myriad formulations exist, making the selection process something of a mining expedition. All of them are considered safe, with just a few reported side effects, including blurred vision, ocular discomfort and foreign body sensation.1-3
Although relatively few trials compare formulations, a 2016 Cochrane review found no evidence of any difference in efficacy or side effects when comparing different artificial tear formulations.2 However, limited data on lipid-containing artificial tears existed at the time of the review, and more recent research may affect the findings.2
With little to differentiate the options, at least superficially, selecting the right one can be intimidating, and patients, if left unguided, are likely to make misinformed product decisions that could impact the therapy’s efficacy.
Here, dry eye experts weigh in on the many artificial tears currently available, which options are best for certain dry eye patients and when to consider switching from one type of tear to another.
The Building Blocks
Artificial tears have both active and inactive ingredients that can impact a patient’s treatment success. Some patients have sensitivities to certain ingredients, and some formulations may be more compatible for certain types of DED, says Jennifer S. Harthan, OD, professor and chief of the Cornea Center for Clinical Excellence at Illinois College of Optometry, Illinois Eye Institute.
 |
|
The ingredients of an artificial tear may impact its efficacy and the patient’s comfort. Click image to enlarge. |
“Patients often view artificial tears as interchangeable, and it’s important to make a specific recommendation to them based on the type of dry eye disease they have and educate them on the differences,” she explains. Treat artificial tears as a prescription. Prescribe them for the specific condition that the patient has, she adds.
Artificial tears are comprised of two main active ingredients: demulcents and emollients.
Demulcents. These are usually a water-soluble polymer that helps to protect and lubricate the mucous membranes of the eye. Most commonly used in this category is carboxymethylcellulose, which increases the viscosity of tears and has mucoadhesive properties that allow for longer corneal coverage, explains Cecilia Koetting, OD, of Norfolk, VA.
Along with carboxymethylcellulose, another common demulcent is hydroxymethylcellulose. Some of these types of demulcents can be found in Refresh Tears (Allergan), TheraTears (Akorn) and Retaine (OcuSoft), Dr. Harthan says.
Propylene glycol, polyethylene glycol and glycerin are other common demulcents. Some of these can be found in Systane (Alcon), Blink (Johnson & Johnson Vision) and Soothe (Bausch + Lomb), according to Dr. Harthan.
Demulcents are sometimes used alone or in combination of up to three, explains Suzanne Sherman, OD, assistant professor of optometric sciences and director of optometric services in the Department of Ophthalmology at Columbia University Irving Medical Center.
The drops range in demulcent concentrations of 0.2% to 1%. The higher the percentage, the more viscous it is and the greater the transient blur, Dr. Sherman adds.
“It’s thought that the higher-concentration drops remain on the eye longer to provide prolonged relief.” explains Dr. Sherman. “If a patient complains of too much blur from their artificial tears, you could look for an alternative with a lower concentration.”
One Piece of the PuzzleDED is a chronic, multifactorial disease, and patients may have varying degrees of signs and symptoms based on the underlying etiology, explains Dr. Harthan. She suggests using a standardized symptom questionnaire at baseline and at follow up exams to assess treatment effects. Additionally, a complete dry eye evaluation should be done to determine disease severity and which management options are best suited for each patient. “Artificial tears are often not sufficient treatment alone and are commonly used in combination with other therapies. It’s important to consider what long-term, specific treatments are needed to target the underlying disease process for each individual patient,” explains Dr. Harthan. “Patients also experience flare-ups throughout the course of their disease. Education is critical for patients to understand their disease and enhance compliance with treatment.” “Artificial tears shouldn’t be seen as the primary treatment of DED for most patients, but as a tool for temporary relief of DED symptoms,” Dr. Koetting adds. “Patients should be evaluated for underlying causes of dry eye and appropriate treatment initiated concurrently.” Dr. Koetting won’t typically start with an artificial tear if a patient has identifiable DED but will instead start to treat the underlying problem. “The patient can supplement the medication with an artificial tear as needed,” she says. |
Emollients. Lipid-containing eye drops, formulated as emulsions, are growing in both availability and popularity, likely due to the increased attention being paid to meibomian gland disease (MGD) and lipid deficiency.1,4,5
Emollients are a fat or oil found in both tears and ointments. Most artificial tears use mineral oil, castor oil or flaxseed oil. They are used to increase the lipid layer thickness, help stabilize the tear film and reduce evaporation. They are typically classified based on the size of the oil droplets: macroemulsions, microemulsions and nanoemulsions, Dr. Koetting says. The size of the oil particle and concentration vary depending on the formulation and can affect the emulsion stability and bioavailability.
Emollients are important ingredients to look for when MGD is an underlying cause of DED, adds Dr. Harthan. However, most emollients added to artificial tears create an emulsion that requires some products to be shaken before instillation. It’s important to fully understand the specifications for each separate artificial tear, Dr. Harthan explains.
Artificial tears containing emollients include Systane Balance (Alcon), Systane Complete (Alcon), Systane Nighttime (Alcon), Refresh Optive Advanced (Allergan), Refresh Optive Mega-3 (Allergan), Refresh PM (Allergan), Soothe XP (Bausch + Lomb) and Retaine MGD (OcuSoft), Dr. Harthan says.
A slew of inactive ingredients are often what set individual drops apart from each other and include preservatives, buffers, emulsifiers, electrolytes, viscosity-enhancing agents and osmo-protectants.
Preservatives. Many artificial tears that come in a multi-dose bottle contain preservatives designed to decrease the growth of bacteria once the bottle has been opened. Commonly used preservatives include benzalkonium chloride (BAK), polixetonium, polyquaternium (Polyquad) and OcuPure, in addition to sodium chlorite, which is considered a less harsh preservative, Dr. Sherman says.
The most common preservative in ophthalmic drops is BAK, but it can be detrimental to the ocular surface as it decreases goblet cell density, delays wound healing, damages corneal nerves and disrupts corneal and conjunctival cells, Dr. Harthan explains.
One alternative to BAK, Polyquad, may be less toxic to the ocular surface for some patients, Dr. Harthan adds.
Preservative-free options generally have fewer additives and commonly come in single-dose vials.
Dr. Sherman considers switching to a preservative-free drop if a patient tends to have chronic allergies, sensitive skin, if they report mild-to-moderate stinging or irritation from non-preservative free formulations or if they need to use the drops more than four times per day. Other considerations would be for individuals, such as glaucoma patients, who are on other topical eye drops that contain preservatives.
In addition, Dr. Harthan considers recommending a preservative-free drop for postoperative cases, those with moderate-to-severe DED, any patient using artificial tears more than four times a day and contact lens wearers. A recent report found that artificial tears and rewetting drops, with or without preservatives, are safe and effective when used before, during or after contact lenses wear, although the author recommends using preservative-free options whenever possible to avoid eye irritation.6
Clinicians should also take note whenever a patient says they are using a daily regimen of artificial tears. These patients should receive a more thorough dry eye evaluation and are likely candidates for escalated therapy.1
“In my opinion, there is not a single patient who wouldn’t benefit from using preservative-free versions of artificial tears,” adds Dr. Koetting. “Even in patients who aren’t known to have sensitivity, when used in high volume, the preservatives can cause corneal damage, furthering their DED.”
If frequent use of preservative-free artificial tears is cost-prohibitive for patients, consider recommending a drop with a preservative that has a demonstrated safety profile, not BAK or thimerosal.
 |
|
This patient with moderate to severe gland loss would do well with a lipid-containing eye drop to help supplement the depleted lipids in the tear film. Click image to enlarge. |
Other ingredients. The buffers and electrolytes within most artificial tears have been adjusted to mimic the pH and osmolarity of the tear film, which can be important for comfort and to avoid stinging upon installation. “Patients may have burning or stinging with certain artificial tears if the pH of the drop doesn’t align with their own tears,” Dr. Harthan explains.
If a patient has burning or stinging with certain artificial tears, it could be due to the preservative or it could be due to the pH or osmolarity of the artificial tear. With a full understanding of artificial tear ingredients, clinicians can help patients choose the right product to enhance comfort, maximize efficacy and minimize toxicity to the ocular surface, Dr. Harthan adds.
Normal tear pH is around 7.4 and the “comfort zone” is about 6.6 to 7.8.7 Although manufacturers don’t advertise the pH in their products, making it hard to find, most artificial tears have a pH between 7.0 and 7.6.7
The physiologic pH of tears is well understood, but the impact of DED on tear pH is less clear, says Meaghan Horton, OD, who practices in Cincinnati. “Tear pH is not a diagnostic criterion for DED and is not routinely measured in clinic,” she explains.8 “Some studies show a small alkaline shift in dry eye patients, but the amount was small and has not been validated as clinically relevant.9,10 Ocular discomfort such as burning and stinging can result from use of solutions with pH that significantly differs from the pH of the precorneal tear film.
TheraTears has been shown to be more alkaline than most artificial tears and would be a good first choice for a patient with significant complaints of stinging on instillation, according to Dr. Horton.11,12
The 2017 TFOS DEWS II report emphasized that tear film osmolarity is central to the pathophysiology of DED as a biomarker of tear film homeostasis.8
“What needs more research is which type of artificial tear, and its relative properties of osmolarity, can impact the osmolarity of the tear film in dry eye patients,” says Dr. Horton. “We know that tear osmolarity changes parallel improvements in the signs and symptoms of DED, but there is limited data available that directly correlates this improvement with a particular type of artificial tear.”
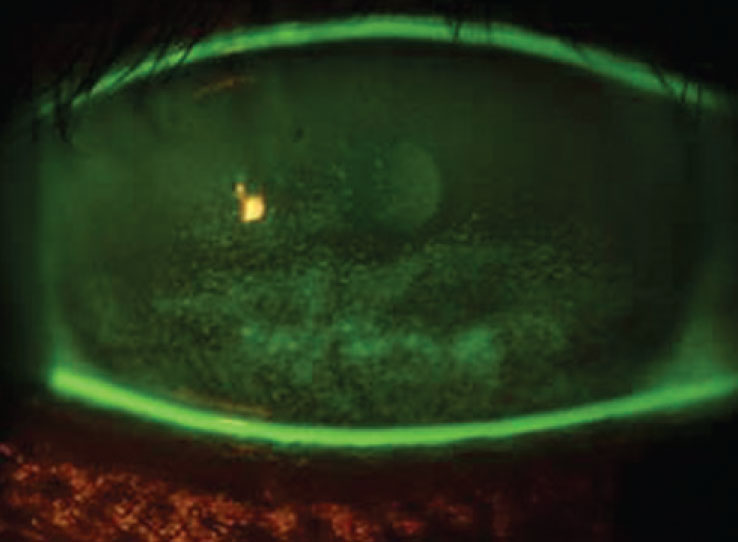 |
|
Sodium fluorescein staining in a patient with dry eye and exposure keratopathy. Patients with severe dry eye may do better with a viscous artificial tear, gel or ointment. Click image to enlarge. |
Patients with an osmolarity of up to around 295mOsms/L would be candidates for most artificial tears of low viscosity if they are using the lubricant infrequently or for episodic symptoms, explains Dr. Horton. Patients at 317mOsms/L or more, signifying moderate disease, should be on anti-inflammatory medications, and the clinician should consider artificial tears with osmoprotective agents, she adds.
“In general, artificial tears should be pH neutral and iso or hypotonic. This would mean a pH very close to 7.4 (may have better comfort profile if slightly alkaline to 7.4) and a hypo or near iso-osmolar quality,” Dr. Horton advises.
Glycerin and trehalose are just two examples of osmoprotectants that have demonstrated in vivo protective effects on desiccated epithelial cells.13,14
Trehalose, found in Refresh Optive Mega-3, is an additive designed to help stabilize cell membranes, while sodium hyaluronate, a glycosaminoglycan, is an ingredient in both Blink and Oasis Tears (Oasis Medical) to enhance viscosity, thereby increasing lubrication to the ocular surface, Dr. Harthan says.
Additionally, hydroxypropyl-guar (HP-guar) is found in Systane artificial tears and helps keep the demulcent on the eye longer, she adds. HP-guar is a polymetric thickener that combines with the two demulcents in Systane to form a low viscosity gel that activates as it interacts with the ocular surface, changing the pH.15
Also new to the field is Refresh Optive Repair (Allergan), a drop that contains both carboxymethylcellulose and sodium hyaluronate.16 This option is said to offer osmoprotective benefits that safeguard the health of epithelial cells against hyperosmotic stress.16
How to Choose
When selecting an artificial tear for a patient, clinicians must consider several factors, including efficacy, duration of relief, ease of installation, viscosity, type of dry eye disease targeted and how a patient will be impacted by the amount of blur a drop may cause, Dr. Harthan suggests. The artificial tear’s pH and the presence or absence of a preservative are also key factors.
The most important first step is determining the patient’s individual needs based on ocular history and the clinical exam, Dr. Sherman suggests. Only once clinicians understand the type of ocular surface disease the patient has can they determine which type of tear is right, she adds.
MGD. A patient with this form of dry eye may benefit from an artificial tear with emollients to help replace the decreased lipids in the tear film, Dr. Koetting says. Some tears in this category include Systane Balance, Soothe XP and Refresh PM.
Evaporative dry eye. This form of DED is often a consequence of MGD; thus, patients often do well with artificial tears containing emollients in combination with warm compresses, environmental management and acknowledgment of systemic medications, according to Dr. Sherman.
Aqueous-deficient dry eye. Artificial tears are a large part of the treatment for this form, and patients often have their favorite, depending on what’s comfortable for them, she says. Here, frequency is key, she adds.
Unfortunately, if dry eye is severe, the patient will need some kind of anti-inflammatory as well. These are the patients who are put on cyclosporine, steroids and/or serum tears, Dr. Sherman says.
“It’s important to emphasize these tears must be used frequently to see results,” Dr. Sherman explains. Artificial tears are often used in combination with anti-inflammatory agents, punctal plugs and omega-3 vitamins, she says.
 |
|
Patients with MGD can benefit from artificial tears, but they will also need therapies that target the underlying etiology. Click image to enlarge. |
Mixed dry eye. The TFOS DEWS II findings suggest that up to 70% of dry eye patients may have a hybrid of evaporative and aqueous-deficient dry eye.1 At least one artificial tear, Systane Complete, is marketed to help alleviate symptoms from evaporate, aqueous deficient and mixed dry eye.
If a patient has mixed DED, Dr. Sherman will always start with addressing the lid margins, including cleaning them and getting the meibomian glands to the highest functioning potential. Using artificial tears that are helpful for evaporative DED will not worsen the aqueous dry eye condition, she adds.
“Often just improving one aspect of their DED will improve the clinical signs and patient symptoms enough to not have to use prescription-strength medications,” Dr. Sherman says.
Some patients require trial and error when choosing the right drop. “If a patient is sensitive to ingredients, do not select an artificial tear that has the same ingredients. Preservative-free tears are beneficial for many,” Dr. Harthan reiterates.
Disease severity. Along with DED type, the staging will help dictate the artificial tear of choice.
Some products target only one aspect of DED, while others target multiple aspects, significantly affecting efficacy depending on the condition, and severity, in question.
“Patients with more severe dry eye or those with exposure keratopathy may require a viscous artificial tear, gel or ointment,” according to Dr. Harthan.
Another point: Take into account what artificial tears your patient has already tried, as many individuals may have tried numerous tears before they reach your chair.
Unfortunately, selecting a comfortable drop for a patient is often a trial and error process. But if it goes beyond removing preservatives and changing viscosity, “the patient most likely has uncontrolled underlying disease and should have targeted therapy to control surface inflammation and/or osmolarity,” Dr. Horton says.
A Generic Debate
Dr. Koetting typically will tell her patients to avoid preserved generic artificial tears. “Even though the active ingredients listed may be the same as the brand name, it’s the preservatives that sometimes aren’t listed. Most notable is BAK, which can lead to further irritation and corneal toxicity,” Dr. Koetting says.
On the other hand, Dr. Sherman says many patients tolerate generic preserved drops well, and it is important to keep in mind that generic drops are significantly cheaper. “I will not ask a patient to switch to non-generic or preservative-free drops if the patient is accepting the drop well, and the artificial tears are providing sufficient results.”
Time to Switch
If an artificial tear is not well tolerated, Dr. Sherman will recommend the patient change brands.
“We are all different, and we tend to have distinctive likes and dislikes,” she says. “No one artificial tear works for everyone. I often tell patients, ‘You have to try a bunch before you find the one that is the most soothing for you.’”
If the patient has tried a few different drops and reports poor tolerance, it is time to switch to non-generic, preservative-free or medicated drops, she says.
If the artificial tear is insufficient in easing symptoms, the clinician needs to look into why, Dr. Sherman adds. Optometrists needs to question whether they are targeting the wrong type of dry eye or whether the patient may have other underlying conditions such as an autoimmune disorder or MGD that exacerbate their symptoms, she says.
Whatever artificial tear you recommend, first consider the formulations of each specific product and the signs and symptoms of your dry eye patients. All products may look the same at first glance, but when it comes to artificial tears, the devil’s in the details.
1. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. The Ocular Surface. 2017;15(3):575-628. 2. Pucker AD, Ng SM, Nichols JJ. Over the counter (OTC) artificial tear drops for dry eye syndrome. Cochrane Database Syst Rev. 2016;2:CD009729. 3. Downie LE, Keller PR. A pragmatic approach to dry eye diagnosis: evidence into practice. Optom Vis Sci. 2015;92(12):1189-97. 4. Lee SY, Tong L. Lipid-containing lubricants for dry eye: a systematic review. Optom Vis Sci. 2012;89(11):1654-61. 5. Moshirfar M, Pierson K, Hanamaikai K, Santiago-Caban L, Muthappan V, Passi SF. Artificial tears potpourri: a literature review. Clin Ophthalmol. 2014;8:1419-33. 6. Pucker AD. A review of the compatibility of topical artificial tears and rewetting drops with contact lenses. Cont Lens Anterior Eye. 2020;43(5):426-32. 7. Perrigin JA, Morgan A, Quintero S, et al. Comparison of pH values of selected ocular lubricants. Invest Ophthalmol Vis Sci. 2004;45:3913. 8. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15(3):539-74. 9. Khurana AK, Chaudhary R, Ahluwalia BK, Gupta S. Tear film profile in dry eye. Ophthalmol (Copenh). 1991;69(1):79-86. 10. Norn MS. Tear fluid pH in normals, contact lens wearers, and pathological cases. Acta Ophthalmol. 1988;66(5):485-9. 11. Stahl U, Willcox M, Stapleton F. Role of hypo-osmotic saline drops in ocular comfort during contact lens wear. Cont Lens Ant Eye. 2010;33(2):68-75. 12. Dalton K. pH osmolality and viscosity of artificial tears. American Academy of Optometry. 2008. www.aaopt.org/detail/knowledge-base-article/ph-osmolality-and-viscosity-artificial-tears. Accessed September 28, 2020. 13. Baudouin C, Cochener B, Pisella P-J, et al. Randomized, phase III study comparing osmoprotective carboxymethylcellulose with sodium hyaluronate in dry eye disease. European J Ophthalmol. 2012;22(5):751-61. 14. Hovakimyan M, Ramoth T, Löbler M, et al. Evaluation of protective effects of trehalose on desiccation of epithelial cells in three dimensional reconstructed human corneal epithelium. Curr Eye Res. 2012;37(11):982-9. 15. Christensen MT. Corneal staining reductions observed after treatment with Systane. Advances in Therapy. 2008;25(11):1191-9. 16. Allergan Expands Refresh Portfolio With New Refresh Repair Lubricant Eye Drops. Chicago: PR Newswire. 2018. www.prnewswire.com/news-releases/allergan-expands-refresh-portfolio-with-new-refresh-repair-lubricant-eye-drops-300677992.html. Accessed September 15, 2020. |

