At the age of 55, Eric White, OD, knew it was time to come up with an eventual exit strategy. Dr. White has been practicing solo for the past 25 years, and although he didn’t have immediate retirement plans, he realized it was finally time to hire another doctor.
The recent addition of Dr. White’s new associate, Michael Morgan, OD, a former patient Dr. White recruited while the junior doctor was still in optometry school, has given Dr. White the chance to travel and lecture without worrying about coverage.
“I’ve been solo for my whole career, and I realized it’s important to have somebody to cover for me. Also, because of my age, I’m getting to the point where I want to start thinking about slowing down,” he says. The decision clicked when Dr. White found an excellent potential associate he could groom to possibly take over the practice when he’s finally ready to retire.
Whether you’re nearing retirement or looking to see more patients with an already full schedule, there’s much to consider before taking the plunge and hiring an associate.
 | |
| Dr. White, of Complete Family Vision Care in San Diego, with his new associate, Michael Morgan, OD. |
What’s Your Motivation?
Practice management consultant Gary Gerber, OD, from the Power Practice, says the number one motivation a doctor should have in mind when considering taking on an additional doctor is quality of life. Doctors should take into account how hard they want to work, how many hours they want to work and how much they want to be compensated for their work, he says.
“There’s a lot of bad advice out there that dictates you should only bring on another doctor if your practice is grossing X amount of dollars,” he says. Six years ago, Dr. Gerber offers as an example, a prospective client with two young children reached out to him to help with her practice, which was only open 2.5 days a week. The doctor wanted the practice to be more profitable and didn’t want to continue to turn away patients, but she wasn’t willing to work more days.
“The first thing we did was get her an associate,” Dr. Gerber says. “Here’s a little, tiny part-time practice [that needed help], yet most formulas say you need to make $800,000 a year before you should hire someone. She wasn’t even close to that; yet in this case, it was the right decision to hire someone.”
Brian Chou, OD, whose practice brought on a new doctor over a year ago to allow for growth, suggests doctors consider hiring an associate if their schedules are consistently booked beyond a week and there is no further capacity to increase exam volume even with better staff delegation, use of technology or office design changes. “While it’s a good problem to have, patients that can’t get in on a timely basis will go elsewhere, which results in lost potential revenue,” Dr. Chou says.
Another key reason to bring on a new doctor is the potential of additional revenue related to expanding hours or new services, Dr. Chou says. For instance, you could hire someone to work on Saturdays and Sundays, or someone with residency training in specialty areas such as glaucoma, low vision or vision therapy, he says.
This scenario has paid off for Dr. White, whose practice expanded hours and is now open an additional day once a month. However, the biggest asset Dr. White’s new associate has brought into the office is “young blood,” he says. “His generation is coming to see him. Additionally, Dr. Morgan has brought more expertise on the medical aspects that I lack; but in turn, I’m teaching him doctor-driven contact lens dispensing.”
Most doctors focus on the practice income and patient load, but another doctor may bring in a different patient population and give you more time to manage the practice, says Peter Shaw-McMinn, OD, who has served as the chairman of the AOA Practice Management Committee and the Association of Practice Management Educators. “A young doctor tends to attract younger patients. A doctor who specializes in VT, low vision, sports vision or glaucoma may bring in patients you would not normally see,” he says.
One caveat to consider is whether or not hiring additional staff would suffice, Dr. Gerber says. “Most doctors hire associates too soon. What they should probably do is hire more staff before they hire another doctor. They usually pull the associate trigger too early.” In some cases, hiring and training staff to take on some of the duties you are not delegating could be the best solution.
“If everything is aligned and it’s a quality of life decision, and the doctor says, ‘My staff is great, but I really think I need somebody else,’ then it is indeed time to hire another doctor, as long as you understand the reasons why you are making this decision,” Dr. Gerber says.
How Much Should You Pay?
The employed optometrist is typically the highest staffing expense. Therefore, owner-doctors must carefully perform their financial due diligence to make sure all the numbers work, Dr. Chou says. To compensate the new doctor, it’s best to talk with several other OD employers in the community to find the going rate. “In projecting how much revenue will be brought in, keep in mind that the new associate is not expected to produce as well as the established doctor, and that there is also variability from associate to associate,” he adds.
Dr. Shaw-McMinn recommends paying the doctor based on productivity, so the more they bring in, the more they get paid. “Twenty-five percent of gross income is a good start, but that will apply to private pay. For vision plans, it will need to be a higher percentage of professional fees and a variable percentage for add-ons, depending upon the plan,” he says.
The adage, “You get what you pay for,” is true in this case, Dr. Gerber says. “You want someone who is a rock star who is going to represent the practice and go out in the community and market. They’ve got to be pretty amazing people, so pay them more than they can get elsewhere. Find the going rate and pay a little bit more. This way, you can be more selective,” he says.
| More Than a Handshake: Get it Down in Writing You’ve made the decision to bring on an associate, and your new OD has accepted the job. Congratulations, but you haven’t completed the hiring process yet, experts say. Finalizing the employment agreement is the final step, which should be reviewed in most cases by a lawyer, they add. “Definitely don’t cut and paste an agreement from Google; get a real lawyer who knows your state laws to do this for you. There’s a lot of risk if you do it the wrong way,” Dr. Gerber says. Besides the general information on salary, start date, hours and vacation, you may want to consider the following for your employment agreement when taking on a new associate: Non-Compete Clause: Depending on state laws, a non-compete, non-solicitation clause should be included with “reasonable” terms, Dr. Gerber says. “It’s not reasonable to say, ‘If you leave here, you can’t practice within a hundred miles for a hundred years.’” The contract won’t be enforceable if you’re not reasonable, he says. Still, the practice owner needs protection if and when the associate leaves, so the contract should spell out that the associate will not be entitled to patient records, they will not be allowed to contact patients, and they will not be allowed to set up a practice within a reasonable distance or there will be a penalty, says Pamela Miller, OD, JD, DPNAP. Remember to check with your legal counsel as to the appropriate terminology that should be used in your state. Depending on the terminology, the “penalty” may or may not be valid or reasonable, she adds. Spell Out Specifics: The more information you include in the contract, the better. Particulars such as who’s paying for things like CE, insurance and state association dues, as well as the amount of vacation time, should all be included, Dr. Gerber says. Tailor to the Individual: Dr. Miller suggests custom-fitting the contract to the specific employee. “Determine if they are going to be full-time, part-time or fill-in, because there are differences,” she says. If someone is hired on a fill-in basis for a day or two a month, a written contract is not that critical. In these cases, if you prefer to have a contract in place, you can create a working one by going back to e-mail correspondence and including the basics of what was agreed upon and discussed, she says. Future Ownership: Another key component that should be included is whether the new employee is going to buy the practice or work their way from associate to partner or purchaser. “There are different intents. Some employees will never reach that status, so it would be a different contract,” Dr. Miller says. Depending on the expectations, spell these out in the contract. Even if the new associate is not planning currently to buy the practice but is full-time and there is a remote possibility they would take over the practice, language should be included in the employment agreement that the first right of purchase would go to the associate, Dr. Miller says. “If you are bringing in an associate, make sure there is some form of safety protection there, and they have first right of the practice. It will help ease both your mind and that of your associate,” she adds. If the new associate will eventually become a potential owner or partner, you may want to include a life insurance clause, Dr. Miller says. Under these special circumstances, in the event the senior partner dies, the new doctor will have money to buy the practice. Potential of Damages: If you hire, for example, a fill-in doctor and the person doesn’t show up, it may cost you. Staff still needs to be paid and patients will need to be rescheduled. In this case, a damage clause in the contract would cover the senior OD, Dr. Miller says. “The senior doctor can pursue legal action, but it’s really up to the doctor, and the matter would probably be settled in small claims court if the practice owner decided to pursue the matter.” Transparency: The senior doctor needs to be aware of the new associate’s level of licensure, professional liability coverage, whether the doctor has been censored or if their credentials have ever been pulled by a third party, Dr. Miller says. “You also want to know if they were ever accused of Medicare, Medicaid or insurance fraud,” she adds. The doctor should check with their state board of optometry and with their own legal counsel when it comes to these issues, as they can differ significantly from state to state, Dr. Miller says. |
Do You Need to Offer Equity?
Equity may be appropriate for the business-minded OD to incentivize growth, but perhaps not for the OD who’s happy just being a worker-bee and takes no interest in additional responsibilities, Dr. Chou says.
“There’s no reason to give equity to the OD unless you want a partner to assist in managing the practice,” Dr. Shaw-McMinn says. “If you are capable of managing the practice, hire independent contractors to see patients or an employee-doctor.”
For Dr. Gerber, equity should be considered on a case-by-case basis. “The equity gets back to the initial reason you’re hiring a doctor. If you’re hiring a doctor because you want some kind of exit plan in place, then equity probably makes sense. If you’re hiring because you just want to work less, remember there are many doctors who have no aspirations of being a partner,” he says.
Dr. White looks at his new associate as his future and has already discussed Dr. Morgan taking over the practice one day. “We sat down and came up with a five-year plan. I don’t expect him to buy in right away because it’s a marriage. You have to make sure you’re compatible. We are extremely compatible, but I also know he’s in debt up to his eyeballs from school. So right now, I want him to work with me for maybe five more years and then decide if it’s right for him to buy into the practice. But, my thoughts are now that he is going to be my exit strategy, so when I’m ready to retire, by that time, he will have already bought into the practice.”
Do You Need to Expand the Practice?
Hiring a new OD will likely mean your practice can accommodate an influx of new patients. With this in mind, meeting added patient volume also requires additional staff, Dr. Chou says. The rule-of-thumb is that approximately four hours of staff time is required for each hour of optometrist time, he adds.
“Bottlenecks in the office need to be identified, and this can be offset by staggering doctor hours or building out a new exam lane and pre-exam space,” he says.
Adding hours may be the easiest solution. “If you’re not open Saturdays, experiment and be open, for example, on Saturdays or Thursday nights,” Dr. Gerber says.
If you practice in a commuter market, also consider adding earlier hours in the morning, he suggests. Dr. Gerber has clients whose practices open at 6am because they are located in commuter towns. If the senior doctor doesn’t want to get to work before the sun rises, ask the newly hired junior doctor to work from 6am until noon on Tuesdays and Thursdays, for example, Dr. Gerber says.
Can You Keep the New Doctor Busy?
Even when the new associate isn’t seeing patients, you can still keep their schedules productive. Dr. Gerber suggests the owner-doctor build time into the new hire’s schedule for practice building and education. Suggest they work three days a week, but see patients for only two-and-a-half days. “You’ll pay them for three full days, but on that other half day, you tell them they are going to be working on developing the practice.”
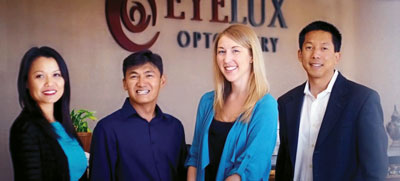 | |
| EyeLux in San Diego recently added a new associate. Pictured from the left is Jacquelin Le, OD; Kelvin Nguyen, OD; new associate Kimberly Michel, OD; and Brian Chou, OD. |
For a new associate with a specialty in sports vision, this could include talking to teachers, putting together a program for high school athletes, or managing the practice’s social media presence.
“They need dedicated time to start building the practice from the first day they start working. It’s a great way to make them busier faster,” Dr. Gerber says.
Are You Ready to Share?
Being a solo practitioner for 25 years, one of the biggest challenges for Dr. White was sharing his long-time patients. Even though Dr. White had known his new associate since Dr. Morgan was three years old, letting Dr. Morgan see his patients wasn’t necessarily easy at first. “I’d look at his schedule and say, ‘Oh, he’s seeing that patient.’ But it’s okay now,” Dr. White says.
Sometimes the transition is made easier by greeting long-time patients in the exam or waiting room and letting them know they are going to have an exemplary experience with the new doctor. This worked for Dr. White when a long-time patient came to see his associate instead of him, since she didn’t want to wait until Dr. White had availability in his schedule. “I went out, gave her a hug, and let her know she’d love Dr. Morgan and she was in good hands. She said she wouldn’t be here if she thought otherwise,” he says.
“Many practice management experts will give you a number to use when your practice can handle another doctor, but I think everyone should have a second doctor in their practice,” Dr. Shaw-McMinn concludes. “There are times you won’t be able to be there, and you can be covered in case of emergency or illness or vacation. Even if you don’t have a full schedule, it’s worth having another doctor there one day a week. While the doctor is seeing patients, you have time to manage the practice and train staff properly. The biggest hurdle is finding someone you are comfortable with.”
