 |
|
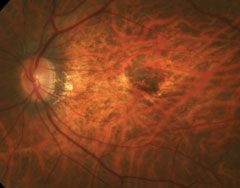
Despite its effectiveness in neovascular AMD, anti-VEGF struggles to reduce CNV in high myopes. Image courtesy of Mark Dunbar, OD. Click image to enlarge. |
Myopic choroidal neovascularization (mCNV) is a serious condition that leads to significant visual impairment and even legal blindness in some cases. Fundus fluorescein angiography is the standard way to evaluate mCNV but is both invasive and time-consuming. It also carries the risk of anaphylactic shock. OCT angiography (OCT-A), on the other hand, is noninvasive and fast. It’s able to scan areas of the retinal tissue and construct microvascular flow maps to evaluate the retinal layers.
Previous studies have reported decreasing macular vessel density in high myopia compared with normal eyes. Researchers say it’s still unclear whether macular vessel density alternates in high myopic eyes with secondary CNV and whether anti-VEGF treatment will impact the vessel density in mCNV eyes. A team in China analyzed the macular microvascular alterations in this patient population as well as the efficiency of anti-VEGF therapy for mCNV with OCT-A. They found that mCNV eyes undergo several changes to the retina and that anti-VEGF was unable to completely eliminate CNV lesions in most cases.
The retrospective study included 123 patients divided into an mCNV group, a high myopia group and a normal group. The researchers measured the following on 3x3mm2 OCT-A images: superficial vessel density, deep capillary density, foveal avascular zone (FAZ) area, A-circularity index (AI), vessel density around the 300µm width of the FAZ region density (FD) and the area of CNV lesions in the mCNV group.
They found that the logMAR BCVA, superficial and deep vessel density and FD of the mCNV group were lower than the two other groups. The superficial and deep vessel density and FD of the high myopia group were also lower than the normal group.
While the FAZ area in high myopic patients was greater than that in normal patients, there wasn’t a significant difference in FAZ area among mCNV and the other two groups. “To some extent, FAZ in mCNV patients may turn smaller,” the researchers wrote. “The mean AI of the mCNV group was statistically greater than the other two groups, which means the FAZ was more irregular.”
They also compared mCNV patients pre- and post-anti-VEGF therapy at one, two, three and six months and found improvements in logMAR BCVA and decreases in central macular thickness, area and flow area of CNV lesions.
The team reported a 50% mean reduction ratio of the lesions. In two cases (5%), they observed lesion regression of 100%. They noted a negative correlation between the CNV lesion area and reduction ratio and the flow lesion area and reduction ratio. “The reduction ratio of the biggest lesion group (>0.5mm2) was less than that of the smaller, but the superficial and deep vessel density, the area of FAZ, AI and FD didn’t change in the mCNV group after anti-VEGF treatment,” they explained.
“Our study further discovered that the superficial and deep vessel density and FD decreased more in the mCNV group,” they said. “Some scholars considered that breaks in RPE-Bruch’s membrane induced by the excessively long axial length develop lacquer cracks which facilitate ingrowth of neovascularization. We guess that the excessively long axial length in mCNV caused lower vessel density.” They added that choroidal ischemia upregulation of VEGF factors is also a potential pathogenesis of mCNV.
“Decreasing superficial and deep vessel density and FD may have the same effect on VEGF,” the researchers continued. “However, there was no significant difference between the superficial and deep vessel densities and FD in the mCNV group before and after treatment. The alterations in vessel density may have existed before CNV emerged. If this assumption was true, it might mean the lower vessel density indicates a higher risk of mCNV. However, we can’t exclude the possibility of anti-VEGF inefficiency in influencing the vessel density.”
Overall, they found that macular vessel density decreased and that the FAZ became smaller and more irregular in mCNV eyes. “Anti-VEGF therapy is efficient for mCNV but unable to change vessel density and FAZ or eliminate CNV lesions completely in most cases,” they concluded. “The mean reduction ratio is 50.32%, but the bigger mCNV lesions have a lower reduction ratio. Further studies are needed to find new treatments to cure mCNV.”
Mao J, Shao Y, Yu J, et al. Macular density alterations in myopic choroidal neovascularization and the effect of anti-VEGF on it. Int J Ophthalmol. 2021;14(8):1205-12. |

