 |
| Angle widening may help assess patients at risk of glaucoma. |
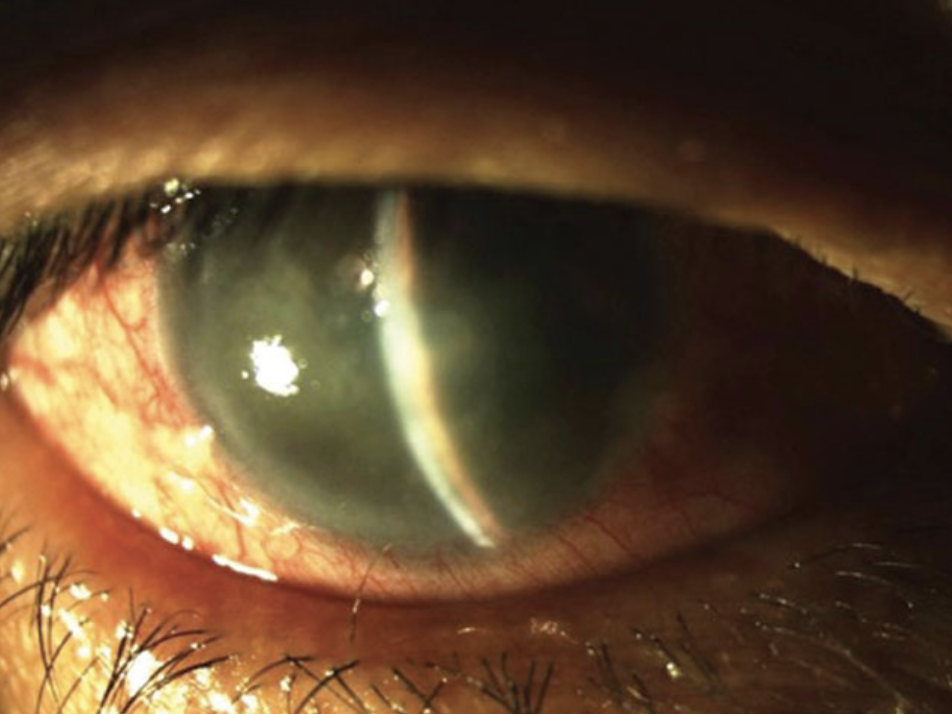
Patients with primary angle-closure disease (PACD) have compromised trabecular outflow, contributing to increased intraocular pressure and glaucoma risk. As primary angle-closure glaucoma (PACG) remains a leading cause of blindness worldwide, it is crucial to understand the risk factors associated with its development in patients with PACD in order to detect the disease and treat it sooner.
Some biometric parameters have been shown to help identify those with PACD at greater risk for glaucoma, including dark-to-light behavior of anatomical structures such as the iris. Since reduced dark-to-light change in the iris area has proven to be a dynamic risk factor in PACD, a group of researchers conducted a study to look further into the determinants of dark-to-light change in angle width and their roles in PACD.
A total of 1,011 participants (22.4% with PACD) were included in the study and underwent an OCT scan in both dark and light settings. The following were calculated for each subject: static dark and light biometric parameters, including angle opening distance (AOD750), anterior chamber width (ACW), lens vault (LV) and pupillary diameter (PD), as well as dynamic dark-to-light changes.
Every biometric parameter differed in dark vs. light conditions for the entire cohort. The strongest determinants of dark-to-light change were changes in ACW and PD. Eyes with PACD had a lower dark-to-light increase in AOD750 than those without (0.081mm and 0.111mm, respectively). ACW was also found to increase in eyes with PACD from dark to light, while it decreased in eyes without PACD. Change in PD was similar in both groups.
“The anterior chamber angle is typically assessed in the dark, whether using gonioscopy or AS-OCT, because on average angles are narrowest and at highest risk of angle closure in the dark,” the researchers explained. “However, the pupil only briefly maintains a static maximally-dilated state under physiologic conditions as pupillary constriction occurs after a brief period of dark adaptation. Therefore, angle widening that accompanies dark-to-light or dark-adapted pupillary constriction could help alleviate angle narrowing and re-establish aqueous outflow in eyes with extensive iridotrabecular contact.”
The team noted that 89.1% of eyes in the study demonstrated greater temporal AOD750 in the light than dark, supporting previous research that suggests the dark-to-light pupillary response promotes angle widening.
“We find that dark-to-light change in scleral spur position, represented by change in ACW and LV, appears to be an important determinant of change in angle width and could contribute to anatomical mechanisms of PACD,” the researchers conclude. They suggested that further studies on the clinical impact of this aberrant dark-to-light behavior will help advance the evaluation of patients with angle closure who are at risk for PACG.
Lifton J, Burkemper B, Jiang X, et al. Ocular biometric determinants of dark-to-light change in angle width: the Chinese American eye study. Am J Ophthalmol. October 19, 2021. [Epub ahead of print]. |

