How many times a day do you see a patient who says their eyes are red, watering or feel tired and find yourself passing out artificial tears like a bank teller passing out lollipops? How often do you do the very same thing the next year?
With nearly 30 million Americans suffering from dry eye, it is more important than ever for optometrists to offer truly personalized medical care and solutions for our patients.1 Here’s how our practice is augmenting our well-established primary care practice with a center for dry eye diagnosis and management.
 |
| The LipiFlow device sits on either side of the closed eyelid to heat any blocked meibum and massage it free. |
Why Specialize?
As Triangle Visions Optometry in Durham, NC, grew from one office to nine since 1974, more and more of our primary care patients came in with complaints of redness, eye fatigue, blurry and fluctuating vision, watering, dryness and epiphora. Like most doctors trying to care for a population of computer users, we employed the full range of our dry eye arsenal. A healthy diet of omega supplements, high quality artificial tears, Restasis (topical cycylosporine 0.05%, Allergan), punctal plugs and daily disposable contact lenses were so commonly prescribed they became drop down menu charting options in the electronic health records. But year after year, patients had the same issues and, even worse, patients who came in with these complaints were getting younger.
With the growing volume of dry eye patients, and with the dismal track record of simple solutions such as artificial tears that every other provider offers, we realized providing more specialized dry eye care could be a true practice builder. Happy patients not only come back, but they tell others about us as well. As we built the dry eye aspect of our clinics, we also saw an increase in medical office visits, and one of our key performance indicators—fill rate—surged.
Gather the Tools of the Trade
In the past few years, clinicians have many more options for dry eye diagnosis and treatment above and beyond artificial tears. Becoming a dry eye center calls for specialized tools that can more accurately diagnose patients with dry eye and meibomian gland dysfunction (MGD), as well as therapeutics that can specifically target each patient’s unique causative factors of their dry eye complaints.
Studies show that approximately 40% of the adult population has clinically significant meibomian gland atrophy, and 86% of clinical dry eye patients have associated MGD.2 To combat this prevalence in our own dry eye center—and to stand out from other local specialists also treating dry eye—we invested in the LipiFlow (Tear Science) treatment device and the meibography imaging LipiView and LipiScan devices (Tear Science). We are still considering adding diagnostic aids such as tear film osmolarity testing to our workup, but due to the high rate of MGD among dry eye patients, we prioritized investing in imaging and treatment solutions for that aspect of dry eye. In addition to the LipiFlow system, several other meibomian gland disease treatment options may be useful to have on hand:
- BlephEx (Rysurg) is an in-office treatment for removing collarettes associated with blepharitis.
- Intense pulsed light treatment has shown improvement in tear break-up time and dry eye symptoms in those with ocular rosacea.3
- MiBo Thermoflo (MiBo Medical Group) is a handheld heating device that targets expression of blocked meibomian glands. As yet, this treatment does not have any peer reviewed published studies discussing its effectiveness.
Currently there are two studied treatments to open blocked glands: manual expression and LipiFlow, the heated pulsation device that gained FDA approval in 2011. Manual expression can be a painful and lengthy process of forcefully expelling blocked meibum from each gland. The LipiFlow device sits on either side of the closed eyelid to heat any blocked meibum and massage it free. The goal of gland expression is to unblock clogged and dying meibomian glands to allow production of the oil layer and halt the atrophy process. While we are careful to educate patients that it’s not a cure for dry eye, studies show that 79% of patients undergoing LipiFlow have improved dry eye symptoms just one month after treatment.4
 |  |
| Hands-on training gives staff a better understanding of the LipiScan (left) and LipiView (right) technology, and personal experience with the devices means they are better equipped to answer patient questions. | |
In addition to gland expression treatments, we stock all of the products necessary for keeping glands open and producing. “We no longer advise warm compresses; we specify compresses with Bruder masks,” says Tony Clark, OD, co-owner of Triangle Visions Optometry. “We prescribe lid cleansing pads (Ocusoft) and will combine that with Hypochlor spray (hypochlorous acid 0.02%, Ocusoft) for patients with more severe blepharitis or Demodex when necessary. We do not simply say, ‘take supplements;’ rather, we specify BioTears (Biosyntrx) or HydroEye (ScienceBased Health) supplements, which combine omega fatty acids with anti-inflammatory agents such as vitamin D and turmeric. The heightened levels of technological advancement, coupled with the higher quality in available products, will equal greater levels of dry eye treatment success.” The HydroEye study showed statistically significant improvements in the dry eye symptoms and signs—including OSDI score, tear break-up time and Schirmer’s score—of post-menopausal women with its formula of black currant seed and fish oil at 12 and 24 weeks of use.5
The FDA approval of Xiidra (lifitegrast ophthalmic solution 5%, Shire Pharmaceuticals) will add yet another treatment option to our armamentarium. Gaining FDA approval in July 2016, Xiidra is a twice daily eye drop that showed statistically significant improvement in inferior corneal staining and a subjective dry eye survey score at both six and 12 weeks of treatment.6 Stimulating tear production and reducing inflammation is essential in keeping most dry eye sufferers comfortable, even after their meibomian glands are functional again. Having Restasis, and now Xiidra, brochures and prescribing information ready in office helps us discuss with patients how to use the medication properly to ensure they understand these prescription medications are not simple rewetting drops. We also walk through potential insurance hurdles they may encounter at the pharmacy to increase the chance they will get the medication filled instead of becoming confused or frustrated and walking away without treatment.
Get Staff On Board
Investing in the technology to make our dry eye center successful was no easy undertaking, and it was just one part of the process. The other crucial aspect, time outside of patient care hours for staff and doctor training, adds up. We had to train our technicians on taking images and performing the treatment itself. They needed to feel comfortable explaining these devices to patients and answering questions about the treatment—and dry eye in general. Front office staff learned how to explain the procedure and some basic information about dry eye to help facilitate questions during phone calls.
Along with staff training, all clinicians learned how to identify ideal candidates for treatment, interpret their meibography images and then educate them on their unique dry eye disease and the keys to successful treatment.
 |
| Patients often resist MGD treatment, even with high quality images such as this, showing signs of disease (in this case, severe truncation) in their glands. |
Patient Education is Key
When it comes to keeping patients informed, using meibography imaging to start the discussion about dry eye has transformed the way we connect the disease symptoms and treatment for patients. It’s one thing to point to a diagram of a meibomian gland on a wall; it’s another to show patients their own meibomian glands and let them see the obvious damage.
“I find that the most remarkable moment for patients is when I show them what ideal, healthy glands should look like,” says Adrienne Bender, senior optometric technician who performs treatments and meibography imaging. “Then I show them their own glands. The symptoms they were telling me about when I took their case history was evidence this issue had been there all along, but physically seeing their glands damaged is the most vital and visible proof of a need for change for the patient.”
Communicating the need for treatment even before symptoms present is essential to caring for patients with dry eye, but it is also the biggest challenge clinicians face when starting a dry eye center. Patients often resist treating MGD, even with high-quality images proving their glands are showing signs of disease. Like most dry eye sufferers, the intensity of each patient’s symptoms is highly variable. Some patients with severe gland disease have very few symptoms, but if their glands are already dysfunctional, they will eventually present with symptoms—presymptomatic, not asymptomatic, we say. In these instances, patient education is especially important. We ensure patients understand if they wait to treat MGD only after symptoms arise, the glands could be so damaged not even the latest innovations can help.
“I like to refer to LipiFlow treatment as ‘an oil change for the eyes,’” says Ms. Bender. “We help rid the eyes of the old, congealed oil, and the body does the rest.”
Another hurdle for patients is cost. Treatment can be expensive, and currently no insurance plan covers the newer modalities. Communicating costs takes sensitivity, but we discuss budgeting options with patients, such as setting aside flex spending money, to help. If we allow the glands to permanently atrophy, no treatment can grow them back, so we always educate that we have a time-sensitive window where treatment will be effective. If we know the meibomian glands are nonfunctional, no other treatment for dry eye will be effective—just a waste of money—until we get the glands working again. Heather Hildebrand, OD, likens her discussion of treating MGD early to intervening for any other chronic degenerative disease.
“Imagine if I could tell a patient who feels fine at today’s exam that we see signs they will get rheumatoid arthritis in the next few years,” she says. “We have a treatment we can do now that will prevent them from suffering from the symptoms of rheumatoid arthritis. What patient wouldn’t want us to help?”
Prepare for Ongoing Care
Doctors and staff know treating MGD isn’t the end to managing dry eye—it’s just the beginning. After treatment, we prescribe each patient a daily regimen to prevent the glands from reblocking and to treat any additional aqueous deficiency or other causes of dry eye symptoms.
We schedule a medical office visit four to six weeks after treatment for every patient to reassess gland expression and discuss any necessary changes to the patient’s daily treatment regimen. These are just like any other dry eye visit and take 10 to 20 minutes, depending on the patient’s needs. We set aside appointment times for medical or contact lens checks to avoid competition with comprehensive exam slots.
Although patients may ask to get their glands imaged again to see their improvement at this follow-up visit, meibography images will look identical both before and after treatment. The only way to assess success is with gland expression; blocked glands won’t express prior to treatment; afterwards, gentle pressure should show expulsion of clear meibum.
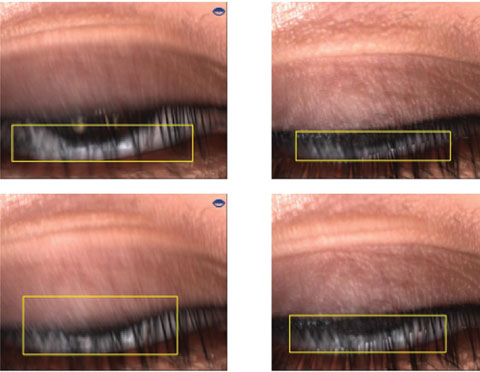 |
| Imaging can help clarify underlying causes of clinical symptoms, such as incomplete blink, as seen here. |
Clinical Extras
One of the most important prescriptions we write after gland expression treatment is blinking exercises. A significant number of patients with advanced meibomian gland disease are long-hour computer users. Staring at screens all day not only slows blink rate, but programs users to take incomplete, partial blinks.7 We have noticed a large number of patients with severe gland atrophy have as much as 100% partial blinking rates. If patients never fully close their eyelids, the meibomian glands do not express, and the meibum stays inside the gland, clogging and hardening until a blockage becomes permanent. We prescribe a free blink training app to help teach patients a normal blink motion and educate them to follow the 20/20 rule.8 Every 20 minutes, break to blink for 20 seconds.
Treating MGD alone can’t make a dry eye center. Reports suggest 14% of all dry eye suffers have aqueous deficient dry eye and roughly 36% of dry eye sufferers have both evaporative and aqueous deficient dry eye, referred to as mixed mechanism dry eye.4 Treating patients with mixed mechanism dry eye requires a multifactorial approach. Our strategy is to attack dry eye from the outside in, starting with eyelid disease by treating any active blepharitis or Demodex infections. Then we address meibomian gland health and inspissation. Once the glands are functional and healthy, we focus on aqueous production and goblet cell health. This approach ensures the surface layers of the tear film are functioning properly before we try to improve the interior tear film layer—if the tear film evaporates right off the surface, all of your work on aqueous production will likely be less effective. Some patients who undergo successful meibomian gland treatment still have break-through dry eye symptoms and will need aqueous and goblet cell function maximized.4 We reach for clinically proven aqueous deficient treatments such as Restasis and even punctal plugs for the right patient, and we now have Xiidra to add to our arsenal.
Getting the Word Out
Treating patients successfully and relying on word of mouth for building a dry eye practice is a tried and true path to success; but in today’s world, word of mouth travels a lot faster if your patients do it online and through social media. Our marketing strategy for the new dry eye center is a mix of both online and more traditional forms of advertising to reach patients of every age cohort that may be affected by dry eye.
“We have seen excellent success utilizing targeted email blasts to existing patients that we’ve flagged during their routine exams as someone suffering with dry eye symptoms. We incorporate a variety of videos and free quizzes to help connect their symptoms to the disease condition and our treatment options,” says Caleb Clark, Triangle Visions’ marketing director. He uses sponsored Facebook ads and Google Adwords to target local patients researching dry eye or the related symptoms online. On our website, a short dry eye questionnaire pops up to help get patients thinking about their eye exam differently.
“It’s not just going to be about their new glasses prescription; our doctors will be talking about how your eyes feel and how we can help improve that too,” says Mr. Clark. “It creates a value to our eye exam that separates us from area providers who are just focusing on traditional glasses and optical needs.”
“I’m also excited to get our toes wet with traditional media,” says Mr. Clark. “The demographic who still reads the newspaper is also the demographic most likely to struggle with dry eye issues. We’ve discussed tying in traditional media advertising with a free screening event for the senior community, and I think that has immense potential to positively impact both our local community as well as our business.”
Building Success
Changing with the times has always been a key to success, but knowing how to change can be challenging. We’ve all heard the same drums beating for dry eye for years now. ‘Become a dry eye center for excellence; it will save lives, promote world peace and make you rich!’ Forgetting the hype, here’s what we know: an enormous percentage of patients in every primary eye care clinic in America has MGD or dry eye syndrome.
With new technology and new treatment options, we can help improve our patients’ health and function in ways we never could before. In so doing, we also develop another vertical revenue column for our practice. It takes some work and focused energy, but it is doable. Anything that can benefit both our patients and our bottom line is a bit of a no-brainer.
There is no silver bullet in treating dry eye, prompting frustrated doctors and patients to reach for the ineffective simple solutions we’ve been using for years. But with new diagnostic tools we can pinpoint the underlying causes of each patient’s dry eye symptoms and make a specific plan of action. We know more about dry eye today than ever before, and as more Americans suffer from dry eye due to diet, lifestyle and digital device use, we are better equipped to offer solutions in our exam chair.
Dr. Jennifer Lyerly is an associate at Triangle Visions Optometry in Cary, NC. She is the founder of eyedolatryblog.com, an eyecare education blog, and cohosts the Defocus Media optometric industry podcast.
|
1. Sullivan DA, Hammitt KM, Schaumberg DA, et al. Report of the TFOS/ARVO Symposium on Global Treatments for Dry Eye Disease: An unmet need. Ocul Surf. 2012;10:108-16. 2. Nichols KK, Foulks GN, Bron AJ, et al. The international workshop on meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci. 2011;52:1922-9. 3. Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; A 3 year retrospective study. Photomed Laser Surg. 2015;33(1):41-6. 4. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous deficient and evaporative dry eye in a clinic-based patient population. Cornea. 2012; 31(5):472-8.Lane SS, et al. A new system, the LipiFlow, for the treatment of meibomian gland dysfunction. Cornea. 2012;31(4):396-404. 5. Sheppard JD Jr, Singh R, McClellan AJ, et al. Long-term supplementation with n-6 and n-3 PUFAs improves moderate-to-severe keratoconjunctivitis sicca: A randomized double-blind clinical trial. Cornea. 2013;32:1297-1304. 6. Shire Pharmaceuticals. Xiidra package insert. Lexington, MA. 7.Portello JK, Rosenfield M, Chu CA. Blink rate, incomplete blinks and computer vision syndrome. Optom Vis Sci. 2013; 90(5):482-7. 8. Korb Blink Training App. Available at https://itunes.apple.com/us/app/donald-korb-blink-training/id941412795?mt=8. |

