The Tear Film and Ocular Surface Society’s 2017 Dry Eye Workshop II defined dry eye disease (DED) as a multifactorial disease with symptoms of discomfort or visual disturbance, and tear film instability with potential damage to the ocular surface. The disease is accompanied by increased tear film osmolarity and inflammation of the ocular surface.1,2 While osmolarity has been a part of the dry eye definition for more than 10 years, it has become increasingly important in clinical practice as more research highlights its utility for diagnosing and monitoring DED.1,2
Objectively, research into hyperosmolarity’s potential effect on the epithelium and nerves shows tear instability is associated with ratings of discomfort and symptoms of burning and stinging.3 Subjectively, tear film osmolarity is an appealing test because it offers a numerical value for dry eye—something most other DED tests lack. Here, we explore what osmolarity is, how it affects the eye and its value in DED diagnosis and management.
 |
| Fig. 1. The TearLab Osmometer is currently the only device clinicians can use in the United State to measure tear film osmolarity. Image: Srihari Narayanan, OD, PhD; I-Med |
Osmolarity 101
A simple measure of solid particles in a solution, osmolarity is an objective measure of the salt concentration in a patient’s tears. Scientifically, it is defined as the concentration of an osmotic solution when measured in liters of the solution. Changes in osmolarity are due to fluctuations in water content, not tear composition specifically—the balance of proteins, lipids and mucins in tears remains stable.4 Hyperosmolarity, whether due to an increased evaporation rate or a reduction of tear secretion, is indicative of reduced aqueous levels.5 Tear film hyperosmolarity stimulates epithelial cell death, which then initiates an inflammatory cascade and leads to proinflammatory cytokine production, cell death via apoptosis and loss of goblet cells.6-10
Research suggests proinflammatory mediators and other sources of desiccating corneal stress stimulate compensatory reflex lacrimal tear secretion via the corneal trigeminal nerves.11 Goblet cell loss also leads to a decrease in mucin production and subsequent tear film instability.12 Increased evaporation resulting from this reduced mucin production may then result in a hyperosmolar state.
In addition, neurogenic inflammation may also play a significant role in the onset and chronicity of ocular surface inflammation and dry eye. This inflammation is produced through the release of neuromodulators when an eye is exposed to pathogens or mechanical disruption, which can cause the release of polymorphonuclear leukocytes into the tears and the intervention of systemic immunity.13
Also, a subsequent loss of corneal sensitivity could further decrease lacrimal production and exacerbate disease severity.1,11
 |
| Fig 2. The I-Pen Tear Osmolarity System is another device currently in use in other countries and on its way to the US market soon. Image: Srihari Narayanan, OD, PhD; I-Med |
Testing, Testing… 1,2,3
The commonly used instrument to measure tear osmolarity, TearLab’s osmometer, uses a micro-electrode to measure the electrical impedance in a tear sample (~0.2 microliters); the electrode is designed to reduce potential reflex tearing, as it avoids direct contact with the ocular surface and collects the tear fluid by passive capillary action (Figure 1).14 The tears are collected at the outermost area of the lateral tear meniscus to minimize the risk of injury to the cornea. Studies show the accuracy differs by only 2mOsm/L in both normal and dry eye patients.14 The instant result, after the tear sample has been collected, also minimizes the level of tear evaporation.14,15 Researchers have found tear osmolarity values are consistent when testing up to four readings taken one to 15 minutes apart.16,17
The I-Pen tear osmolarity system (I-Med Pharma) is another device designed to detect and indirectly measure tear film osmolarity values (Figure 2). It uses single-use sensors to gather a sample with approximately two to five seconds of contact with the tear-soaked palpebral conjunctiva, rather than a liquid sample (Figure 3). This may be considered a benefit in cases of severe dry eye when a tear sample may be difficult to obtain. The I-Pen is designed to measure the electrical impedance in the tear-soaked tissues 192 times in less than five seconds and then calculate the osmolarity of the tear film. It has received regulatory approval in Columbia and Argentina and is now available in five countries in South America. The Food and Drug Administration issued an Acceptance Review Notification for the device’s 510k submission in December 2017, and distribution in the United States is expected after 510k approval sometime in 2018.18
During a dry eye evaluation, clinicians should remember to perform tear osmolarity before any other test, such as vital dye ocular surface staining, to avoid introducing a solution or creating reflex tearing, which could alter the osmolarity. Contact lenses do not have to be removed before this test. TearLab also recommends not collecting tear fluid from a patient within two hours of their use of eye drops, topical medications, face lotions or eye makeup remover, as all of these may trigger reflex tearing.
Systemic and Ocular AssociationsA number of studies show increased osmolarity in various ocular conditions other than DED, such as ocular graft-vs.-host disease (GVHD), Sjögren’s syndrome (SS), pterygium, thyroid ophthalmopathy, ocular mucous membrane pemphigoid and in patients using topical glaucoma medications and in association with air pollution.1-10 One study found tear osmolarity increased in patients with chronic ocular GVHD and was significantly correlated with tear break-up time (TBUT) and, to a lesser extent, Schirmer test values and Ocular Surface Disease Index (OSDI) scores.1 Another study also reported a significant positive correlation between tear osmolarity and corneal staining and OSDI scores, and a significant negative correlation between tear osmolarity and Schirmer value and TBUT.1 In primary SS, research shows a positive correlation between mean osmolarity and OSDI score and fluorescein ocular surface staining; a negative correlation between mean osmolarity and Schirmer test without anesthesia; and no correlation between osmolarity and TBUT.5 Diabetes mellitus is associated with hyperosmolarity as well, particularly based on the duration of the diagnosis.11,12 Research suggests the mechanism is a decrease in aqueous secretion as a result of microvascular damage in the lacrimal gland and corneal nerve.12 Dry eye symptoms are common in patients with Graves’ disease, and one study found ocular discomfort was associated with hyperosmolarity in approximately half of patients with the disease. Increased interpalpebral fissure in patients with Graves’ disease was also significantly correlated with hyperosmolarity.13
|
A Numbers Game
Tear osmolarity threshold values vary from 305mOsm/L to 316mOsm/L, depending on the research.15,16 One study reports that using an osmolarity threshold of 305mOsm/L gave a 98.4% positive predictive value.16 In other studies, a tear osmolarity threshold of 316mOsm/L to 317mOsm/L gave a sensitivity that varied from 59% to 81% and a specificity from 78% to 94%, with a positive predictive value of 85% and a negative predictive value of 74%.19-21 A meta-analysis that used a 316mOsm/L threshold noted that tear osmolarity may be more accurate in the diagnosis of dry eye than lactoplate immunoassay test, Schirmer test and rose bengal testing.19 Studies also show tear osmolarity is influenced by, and correlated with, disease severity.19,20
Currently, most researchers believe the 316mOsm/L threshold better discriminates between mild and moderate-severe dry eye, while 308mOsm/L is a widely accepted threshold.15 Most clinicians identify the 308mOsm/L threshold with diagnosing dry eye, as it appears to be the most sensitive for discriminating between normal eyes and those presenting with early stages of the disease.19 In one study, a tear osmolarity of 308mOsml/L correctly diagnosed severe dry eye 90.7% of the time and normal tear film 81.3% of the time.19 TearLab reliability studies determining diagnostic performance revealed a sensitivity of 81% and a specificity of 80% when using the threshold value of 308mOsml/L.22 Another study reported the coefficient of reproducibility was 39mOsml/L and the coefficient of repeatability was 33mOsm/L.23 The highly variable nature of the tear film may be at play with these relatively large values, which may be due to a small tear film sample in the tear meniscus at that given time. Others show that a variation of 35mOsml/L in consecutive tear osmolarity readings in an individual and an average over three consecutive readings was a reliable indicator of tear osmolarity at a 95% confidence interval.24
Inter-eye tear osmolarity variability can also be diagnostic of dry eye; one study found variability between the two eyes in mild, moderate and severe dry eye patients was 6.9 ±5.9mOsm/L, 11.7 ±10.9mOsm/L and 26.5 ±22.7mOsm/L, respectively.19 Variability also seems to increase with severity, both in inter-eye measurements and repeat measurements in the same eye.19 Using the higher osmolarity value of the two eyes can increase the likelihood of a correct diagnosis. Because the tear film is highly dynamic, a single osmolarity value of the tear meniscus sample should be only one data piece to consider in addition to other dry eye testing.
 |
| Fig. 3. At left, TearLab’s osmometer collects a liquid sample at the outermost area of the lateral tear meniscus. The I-Pen, at right, gathers a sample with approximately two to five seconds of contact with the tear-soaked palpebral conjunctiva. Click images to enlarge. Images: Srihari Narayanan, OD, PhD; I-Med |
Fitting In
Researchers looked at tear osmolarity testing in dry eye patients vs. normal control subjects and even compared it with diagnostic tests already in use, including Schirmer I, fluorescein break-up time, ferning test, lissamine green vital staining, tear clearance, corneal esthesiometry, conjunctival scraping and imprint cytology. Tear osmolarity’s diagnostic performance is promising: research found a highest correlation between tear osmolarity and tear clearance, TBUT and a clinical score; a medium correlation with lissamine green staining, ferning testing, scraping and imprint conjunctival cytology; and a small correlation with subjective symptoms score, tear volume and corneal esthesiometry. Given osmolarity’s good performance compared with other mainstream dry eye testing, particularly in severe dry eye, researchers feel it should be considered a valuable clinical test. Not only can it be helpful in making a diagnosis of dry eye, it can also be used to evaluate the management plan with serial testing on follow-up examinations.16
A review that evaluated the correlation between changes in tear osmolarity, symptoms and corneal fluorescein staining in patients with DED found a statistically significant correlation between changes in corneal fluorescein and symptoms of DED. Interestingly, there was no correlation between the recorded change in dry eye symptoms or tear osmolarity in corneal fluorescein staining. A multivariate analysis revealed that changes in corneal fluorescein staining had a predictive value on symptom changes, whereas tear osmolarity changes did not. Therefore, improvement in corneal staining was associated more with an improvement in patient symptoms than improvement in osmolarity values.25
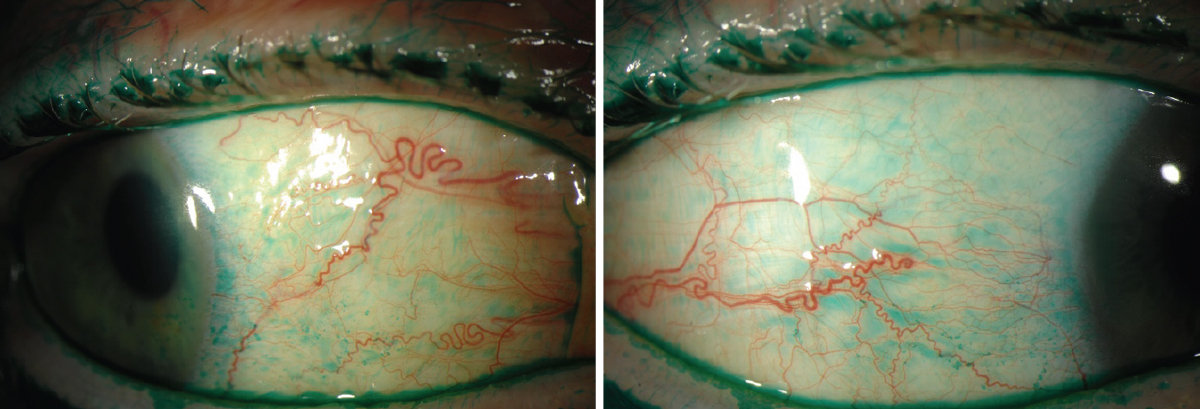 |
| Fig. 4. Osmolarity is a helpful tool to use in addition to other dry eye diagnostics, such as lissamine green staining on the conjunctiva, seen here. Click images to enlarge. |
While tear film osmolarity is a beneficial measurement as part of a dry eye evaluation, it should be used in combination with other testing (Figure 4). In early stages of DED, for example, compensatory mechanisms occur to help maintain osmolar homeostasis, which may result in variable—even normal—osmolarity readings in patients with dry eye symptoms. Examples of compensatory mechanisms include increased blink rate and aqueous tear production.
Periodic osmolarity testing is quite helpful when evaluating the progress of treatment, as most therapies are designed to significantly reduce osmolarity values:
Meibomian gland expression. A single-center review of patients with meibomian gland dysfunction and DED with baseline osmolarity >307mOsm/L reported a statistically significant reduction in mean tear film osmolarity from 317mOsm/L to 306.6mOsm/L after thermal pulsation treatment.26
Topical steroids. For patients with moderate to severe dry eye, topical 1% methylprednisolone QID reduced osmolarity and cytokine levels at four weeks and eight weeks compared with baseline.27
Artificial tears. When evaluating osmolarity values with the use of different artificial tear drops five times daily in patients with moderate to severe dry eye, researchers found the mean tear osmolarity decrease at week 12 was anywhere from -25.7 ±13.1mOsm/L to 33.8 ± 8.3mOsm/L, depending on the brand.28
Tear film osmolarity is quickly becoming an important tool in clinical practice; it’s not only a useful numeric value to obtain as part of a dry eye evaluation, but it’s also great for monitoring treatment progress. With a good understanding of the inflammatory pathophysiology of dry eye, clinicians can appreciate the utility of osmolarity testing and successfully integrate it into their dry eye management plan.
The Influence of External FactorsAny number of environmental stimuli can impact osmolarity, the most well known being smoking. A prospective, case-controlled, comparative study demonstrated that smoking one pack of cigarettes a day caused significantly higher osmolarity values and OSDI scores than nonsmoking subjects.1 Others found acute smoke exposure caused tissue damage associated with increased products of lipid peroxidation and degradation products of the extracellular matrix.2,3 Lipid disruption of the tear film also occurs in smokers, as one study found the lipids did not spread over the corneal surface when the tear interference pattern was analyzed with a DR-1 lipid layer interferometry device.4 Other external factors may have an effect, but research is still divided. For example, controversy exists over whether humidity impacts osmolarity, as the few existing studies show conflicting results. Some studies show a high variability in osmolarity in “normal” subjects exposed to low relative humidity, while others show no increase or variability based on exposure to low humidity.5,6 Research into contact lenses and osmolarity also shows either an increase or no effect on osmolarity with contact lens wear.7-12 One study of 52 women using oral contraceptive pills and contact lenses compared with 45 women not using any form of hormonal contraception, found no significant differences in OSDI and tear osmolarity among the same subject groups.12 However, the researchers did conclude that dry eye symptomatology was worse in the group using oral contraception and wearing contact lenses.12 Ocular surgery may influence tear film osmolarity, but study results depend on the procedure and patient age. One study found tear osmolarity in patients with an average age of 70.83 ± 10.66 increases after cataract surgery.13 In contrast, patients with an average age of 26.2 ± 4.4 status-post refractive surgery did not demonstrate an increase in tear osmolarity.18 Immediately after phacoemulsification, statistically significantly detrimental changes occurred in all dry eye parameters (tear production, evaporation, lipid layer interferometry, osmolarity and corneal sensation) and tear physiology recovered by one month. Corneal sensation, however, did not return to normal values in three months, but a trend towards full recovery was noted. Patients on chronic topical anti-glaucoma medication and post-trabeculectomy patients were more likely to have raised tear film osmolarity and dry eye symptoms, suggesting significant ocular surface disease.14 Researchers note dellen formation proximate to the blebs in 10% of trabeculectomy cases, which they thought was associated with a compromised tear film that has a tendency to break up adjacent to the bleb.15 In addition, antimetabolites (e.g., mitomycin C) compromise the corneal epithelium, which, combined with inflammatory cells, may lead to a poor tear film.16,17
|
Dr. Hessen is a clinical instructor at the Wilmer Eye Institute’s Ocular Surface Diseases and Dry Eye Clinic at Johns Hopkins School of Medicine, where she specializes in ocular surface disease, including autoimmune disorders.
1. The Definition and Classification Subcommittee of the International Dry Eye Workshop. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry eye Workshop (2007). Ocul Surf. 2007;5(2)75-92. |

