 |
A 43-year-old Caucasian male presented to clinic with an irritated, red and teary right eye ongoing for three days. The patient visited a local urgent care clinic with the same concerns two days prior and was prescribed topical gentamicin TID with no improvement. He also indicated flu-like symptoms weeks prior to the onset of his ocular symptoms, which had since resolved.
His entering distance aided visual acuities were 20/20 OD, OS. A slit lamp biomicroscopy revealed 1+ diffuse bulbar conjunctival injection, thick purulent discharge and negative corneal findings with unremarkable sodium fluorescein staining. The diagnosis of acute conjunctivitis was made and the patient was prescribed topical prednisolone acetate QID OD until his follow-up in a week. He was instructed to discontinue the previously prescribed topical antibiotic.
However, the patient returned two days later with complaints of eye pain, decreased vision, light sensitivity and foreign body sensation in the right eye; all of which had progressively worsened since his initial examination. His visual acuities were measured at 20/40 OD with no improvement to pinhole and stable in the left eye. Anterior segment findings were 3+ bulbar conjunctival injection, mild chemosis, trace follicles in the inferior palpebral conjunctiva, diffuse lid erythema and swelling, and multiple small central corneal infiltrates in the right eye (Figure 1). We also observed positive palpable adenopathy on the ipsilateral preauricular aspect of the face, but no evidence of pseudomembranous formation. Based on the clinical presentation and ocular findings, we diagnosed the patient with epidemic keratoconjunctivitis (EKC).
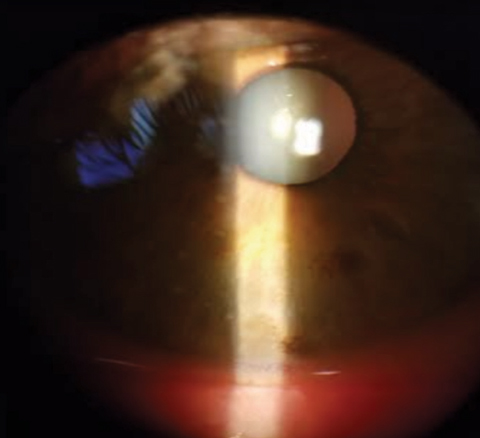 |
| Fig. 1. Multiple small central corneal infiltrates in our patient’s right eye. |
Our Approach
To sterilize the anterior ocular surface from the adenovirus, several drops of Betadine (povidone-iodine 5%, Purdue Pharma) sterile ophthalmic prep solution were instilled into the eye and he was asked to roll the eye around to provide the Betadine access to all conjunctival areas. Betadine drops were also applied to the lash and lid margins and cleaned with cotton swabs under sanitary gloved conditions. A thorough saline solution lavage followed. One drop of a topical anesthetic, Proparacaine (proparacaine hydrochloride ophthalmic solution 0.5%, Bausch + Lomb) and Acular (ketorolac tromethamine 0.5%, Allergan) were used before and after Betadine rinse for ocular comfort. Following treatment, we instructed the patient to continue with the topical prednisolone acetate ophthalmic suspension every three hours in the right eye for two days and apply topical artificial lubricants every hour or two.
Two days later, he exhibited significant improvement in ocular signs and symptoms (Figure 2). The topical steroid was tapered down. The patient remained stable at the five-day follow-up visit with absent ocular signs.
Discussion
Adenoviral infections are common viral conditions that often affect several bodily systems, including the eye. Adenoviruses are non-enveloped, double-stranded DNA genome with multiple serotypes which enter the host nucleus and shed their DNA, resulting in inflammatory response cascades and subsequent infection. The severity and duration of the virus depends on the serotype involved and level of immunocompromise. Upon viral shedding, clinical manifestations become observable for up to 16 days during this incubation period.
The EKC type of ocular adenovirus presentation is highly contagious, and commonly transmits through airborne droplets and hand contact with ocular secretions.1,2 Because of the non-enveloped genetic structure of adenoviruses, they are often impervious to disinfectants and able to survive for weeks on common fomites such as tables, countertop surfaces, desks, doorknobs and towels. Outbreaks are common in winter and summer months and within daycares, schools, military training facilities and professional medical office settings, including optometry.1,2
The presentation of EKC is patient dependent with variable severity, intensity and duration. Mild-to-moderate cases have typical symptoms of conjunctival injection, foreign body sensation, tearing, subepithelial corneal infiltrates and lid edema.
Confirming the diagnosis can be tricky and challenging because ocular symptoms and signs of EKC share similar clinical features as other conditions with allergic, bacterial, inflammatory, contact-related and herpetic etiologies. Therefore, EKC should be a diagnosis of exclusion. An extensive case history and careful ocular evaluation are warranted to rule out other potential masqueraders.2 AdenoPlus (Quidel) immunoassay is a highly specific and sensitive in office detection method that uses conjunctival scrapings and provides “yes or no” results within approximately 10 minutes confirming the presence of an adenovirus.3
Other diagnostic tests include polymerase chain reaction and cell culture combined with confirmatory immunofluorescence; however, these are not readily available.3
Therapies
Currently, the FDA has approved no treatments for adenoviruses.1,2 However, some off-label inexpensive medicine approaches are effective in its management. Because of the highly contagious nature of the condition, hygiene is stressed aggressively to prevent an epidemic. Milder cases respond well to topical artificial tears and cool compresses alone without the intervention of pharmaceutical therapy.1 Topical corticosteroids are effective in the reduction of corneal epithelial infiltrates and ocular relief; however, they are believed to prolong the viral shedding process.1,2 Potential side effects of steroids should be assessed, especially if long-term use is required. In cases that do not respond well to corticosteroids or other approaches, topical tacrolimus 0.03% is a safe alternative option.4 Topical and oral nonsteriodal anti-inflammatory drugs can also aid in ocular pain management and relief.5
Several studies show success with Betadine against adenoviruses.1,6
Zirgan (ganciclovir 0.15%, Bausch + Lomb) has also revealed promising results against adenoviruses.7,8 Other available options include cyclosporin A and cidofovir; however, studies did not find significant reductions or alterations in the infection disease process.9
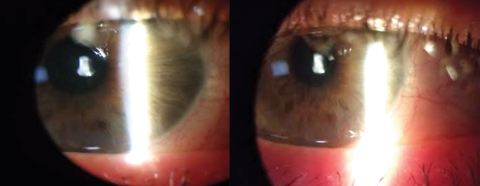 |
| Fig. 2. These images show our patient’s significant improvement in ocular signs and symptoms after two days of treatment. Click images to enlarge. |
Prognosis
Although EKC is a self-limiting and short-lasting condition, some untreated or more severe cases may lead to devastating or permanent effects such as conjunctival or corneal scarring, pseudomembranes, irregular astigmatism, nummular keratitis, periorbital involvement and secondary bacterial infections, all of which become more complex to treat and require more aggressive treatment approaches.2
Adenoviruses are common conditions that medical professionals encounter often. While there are no approved treatment protocols, it is important to make patients aware of the effectiveness of off-label, safe, inexpensive therapies which are underused. Once the diagnosis of an acute EKC presents, aim to eliminate the presence of the viral infection by initiating maximal therapy early in the disease course. Delaying the application of these treatment methods may result in an ineffective or minimal therapeutic response.
Dr. McGhee practices at Chiasson Eye Center and Bond Wroten Eye Clinic in Louisiana.
1. Melton R, Thomas R. Stop EKC with a ‘silver bullet.’ Rev Optom. 2008;145(11):77-81. |

