The pediatric population is underserved in optometric care. For years, federal agencies and educational systems have touted vision screenings as the gold standard in maintaining eye health. Optometrists know screenings are not sufficient to reveal undetected vision problems; in reality, they require a complete workup and, often, comanagement subsequent to their detection. With the integration of the pediatric cohort into eye care via the Patient Protection and Affordable Care Act (PPACA, or ACA for short), millions of children in the United States now have access to comprehensive ophthalmic examinations, that will eventually reveal undetected vision problems.
Call To Action
|
Optometrists will have the chance to make history because of the profession’s unique position to provide greatly needed services. What is the our role within the new care model ushered in by the ACA’s historic passage? Let’s address six key questions.
Has the emphasis on prevention brought more pediatric patients into ODs’ offices?
The premise for the inclusion of the pediatric essential health benefit (EHB) was that it would help reduce the high prevalence of amblyopia—3% to 5% in the United States in some studies—that the ACA highlighted to the nation and health care providers across specialties.1
When the ACA debuted, enrollment numbers were dismal, and those who did enroll were mainly young, single adults. The enrollment of pediatric patients fell short of expectations; however, two years into the program, enrollment numbers are on par with what were anticipated—almost 10 million people of all ages have either signed up for health insurance in state and federal marketplaces under the ACA or were re-enrolled in coverage for 2015.2
It is now more reasonable to expect an uptick in pediatric patients. The implementation of the law was not without its setbacks, so it is only after two full years that the impact of the law on patient coverage can be seen. A poster presented at this year’s Academy meeting showed preliminary data on ACA patient visits in optometric practices (see Table 1).3
Amblyopia patients, who are also taxpayers, may not be able to function in the workforce to the same degree as their binocular counterparts. They may have an aversion to reading and fall behind in school—80% of learning is derived from vision, according to the AOA—or have a higher failure rate in workforce entrance.4
These exact points were made to ACA policymakers by the AOA, and it had a significant impact on their decision to include pediatric comprehensive eye exams as one of the 10 essential health benefits obtained in the plan. In general, amblyopia is very expensive for the government if it is not caught early.
 | |
| The high prevalence of amblyopia was the major reason for the inclusion of pediatric eye examinations into the ACA. |
Over time, with more families participating, we will see an uptick in the number of pediatric patients entering optometric offices.
How serious is the impact of access on pediatric eye health?
Alarming statistics have prompted a call for action in the optometric profession.5 Ten million children in the United States have undetected vision problems, and only 14% of all children have had an eye examination by age six. Only 51% of school-age children ages six to 16 have had a comprehensive eye examination, and more children receive a vision screening than receive a comprehensive eye examination before kindergarten.5,6,7 Of course, unless amblyopia is caught and treated before age 14, permanent visual impairment can occur.8 Aggressive occlusive and vision therapy and accurate refractions, ascertained from a cycloplegic refraction, are needed to ensure that amblyopia is prevented. It is generally known that the earlier that you catch amblyopia, the better—preferably before the age of eight. Optometric and pediatric ophthalmology guidelines recommend first eye exams between the ages of six and 12 months, then again at both three and six years of age.5 The ACA’s inclusion of pediatric comprehensive eye exams thus aims to improve the eye health of the pediatric population with early detection; it works well—almost in concert with the recommended pediatric exam timeline/schedule.
What are some practical applications?
To succeed within the ACA health model, be intentional about opening the doors of your practice to pediatric patients. Here are some tips for better clinical treatment and patient workflow:
• Make your office kid-friendly; have a child-designated area in your reception room.
• Consider having a pediatric examination lane devoted specifically to pediatric patients.
• Always cycloplege pediatric patients in order to obtain the most accurate refraction, and become proficient using lens bar retinoscopy.
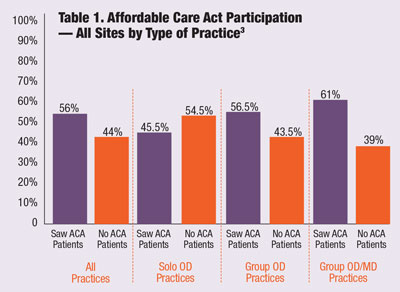 | |
| A 2015 survey polled 125 externship sites in 23 states. Fifty-six percent of sites participated in ACA. Solo OD practices participated at a rate of 45.5%, group practices 56.5% and group OD/MD practices at 61%. Six out of 125 sites participated in an ACO. The survey showed that only a slight majority of surveyed ODs see enrolled patients. |
• Scheduling: Remember that pediatric patients require an initial five to 10 minute evaluation by the doctor and technician. Then they are cyclopleged, which can take up to 45 minutes to obtain maximum dilation. The second part of the exam is the wet refraction and internal health examination. To save time on established patients with no strabismus or near complaints, cyclopentolate 1% can be prescribed for the parent to administer one hour before the yearly appointment or follow-up. The patient comes in already dilated once your initial measurements are obtained.
What can be done to improve care and access?
Three ways that optometry’s access to pediatric patients can improve are as follows:
• Educate other health care providers about the value of pediatric optometric care. Pediatric access to optometry depends on grassroots efforts with other medical professions, institutions of higher education and professional schools. For instance, optometry can reach out to physician assistant schools, the schools of occupational therapy, physical therapy and nursing, as well as community health clinics, to educate these professions on the value of optometric pediatric care. Strategically positioning designated “education key people” in your state can help get the word out about how optometry plays a vital role in accomplishing the goals of the pediatric vision EHB.
• Partner with your state or national educational associations. This can be a great way to increase access to care. Teachers are on the front lines in detecting eye problems linked to students’ learning. For instance, teachers in kindergarten through sixth grade are the ideal group for recognizing vision problems in children, such as convergence insufficiency. Promote the pediatric vision EHB to these organizations so they understand that pediatric comprehensive eye exams are now easily available through the coverage provided by the ACA.
| Online ACA Resources General ACA overview: www.Healthcare.gov/glossary/essential-health-benefits Individual state vision information: http://obamacarefacts.com/vision-insurance State health exchanges: http://obamacarefacts.com/state-health-insurance-exchange |
• Increase awareness of how important and easy it is to access pediatric comprehensive eye examinations through state Medicaid programs. The Medicaid pediatric population in schools sometimes does not take advantage of its Medicaid benefits. Many states provide a yearly comprehensive eye examination for Medicaid enrollees. The challenge is that the enrollees may not realize their benefits cover eye examinations and in some cases their materials, depending on the state’s benefit plan. Reach out to your local school systems to educate parents about the vision health benefits offered by Medicaid for their children.
The details of how to access care can also be found on the state health exchange programs. For information about your individual state, go to www.cms.gov and select “State Marketplace Resources,” or contact your state association. Additionally, it’s essential to work with key people in the legislature and have access to your state Department of Education.
There has never been a better time to hear from us as a profession. Optometrists must continue to be vigilant in our grassroots efforts to ensure the pediatric EHB stays in place and has the opportunity to show its merit.
 | |
| Make your office kid-friendly with a large selection of pediatric frame designs. |
What are strategies for comanaging with pediatricians or pediatric ophthalmologists?
Better communication with pediatricians and pediatric ophthalmologists can easily improve pediatric access to optometrists.
The reality is that most pediatric ocular emergencies come through the pediatrician’s office, and then get referred to pediatric ophthalmology. But there are far fewer pediatric ophthalmologists than optometrists in the nation and the demand for care has increased substantially There are fewer than 500 pediatric ophthalmologists nationwide, which has left the specialty unable to meet the needs of a growing pediatric population. As a result, there is typically a backlog of patients trying to obtain care through a referral to pediatric ophthalmology from their primary care physician. In contrast, 40,000 optometrists are currently in practice nationwide.9 Therein lies the argument for increasing access to care for the pediatric population through optometric practices.
Reaching out to medical schools, pediatric residency programs and pediatric offices is the key to educating physicians on the expertise that optometry offers in the area of pediatrics. Most pediatricians are very uncomfortable even using an ophthalmoscope, and most pediatric residents get less than a month of rotation in pediatric ophthalmology. Pediatricians and ancillary staff are generally very grateful when optometrists reach out to their practices to offer training, correspondence, comanagement and educational tips
Additionally, working directly with the pediatric ophthalmologists in your area can help patients access optometric care. For instance, amblyopia usually requires follow-ups every two to three months in the initial phases of treatment. There is opportunity for shared care between optometry and pediatric ophthalmology in this particular disease process, as well as many other pediatric ocular conditions.
 | |
| The ACA provides the unique opportunity to integrate pediatrics into your practice. |
Intentionally reaching out, being available, educating, training and communicating help the pediatric population gain access to optometric care. There has never been a better time for optometrists to provide care, and the demand is only going to increase. Now is the time to be fiercely intentional about strategically placing yourself as a pediatric-friendly optometric practice, and in doing so, being better positioned for a greater influx of ACA patients.
What common pediatric conditions need to be caught by schools and pediatricians?
• Amblyopia. Affecting upwards of 3% to 5% of the population, it is the single most important reason why comprehensive pediatric eye exams were included as an EHB.
• Refractive error, especially latent hyperopia.
• Retinoblastoma, typically presenting as leukocoria or strabismus.
• Retained foreign bodies.
• Differential diagnosis between optic nerve drusen and papilledema.
• Convergence insufficiency, strabismus and other oculomotor disorders.
• Preseptal cellulitis and lid abnormalities such as chalazion and nasolacrimal duct obstructions.
Optometry is equipped to diagnose and manage or comanage these conditions at a level of excellence that many children are not currently receiving, so it is critical that we engage pediatric patients, ultimately for the child’s benefit.
| Pediatric Eye Care Resources for Optometrists 1. AOA Think About Your Eyes: http://thinkaboutyoureyes.com/about. 2. InfantSee: www.infantsee.org. 3. Your local college of optometry, and the College of Optometrists in Vision Development (COVD): www.covd.org. 4. The Pediatric Eye Disease Investigator Group (PEDIG): www.pedig.net. 5. Pediatric optometrist/ophthalmologists in your local area for knowledge and referrals. 6. Local, state and national associations. |
Final Thoughts
Now is the time to position yourself as a pediatric-friendly practice by incorporating an environment for children in your office. Become intentional about marketing your pediatric skills to schools, hospitals, pediatricians, pediatric ophthalmologists and ancillary health professionals. Finally, take advantage of the many resources available to help improve your skills and your knowledge of the pediatric population. By engaging in pediatric eye care, you will not only help children’s eyes, but their lives as well.
Dr. Elliott is the director of a high volume pediatric ophthalmology practice in Tulsa, Okla. She was 2012 legislative doctor of the year and 2014 optometrist of the year for Oklahoma. She is cofounder of www.take10vision.com and a continuing education speaker.
1. Rainey, AM. What’s New and Important in Pediatric Ophthalmology and Strabismus for 2011. Paper presented at the 37th Annual American Association for Pediatric Ophthalmology Meeting, April 1, 2011; San Diego, CA.2. Armour S. Affordable Care Act Enrollment Near 10 Million. www.wsj.com/articles/affordable-care-act-enrollment-near-10-million-1423070147. Updated 2/4/2014. Accessed October 2015.
3. Ruskiewicz J, Gurwood A. Vision care providers and the and the affordable care act; a snapshot of participation analyzed by one college of optometry’s externship providers. Paper presented at American Academy of Optometry Meeting 2015, October 8; New Orleans, LA. 4. School-aged Vision: 6 to 18 Years of Age. www.aoa.org/patients-and-public/good-vision-throughout-life/childrens-vision/school-aged-vision-6-to-18-years-of-age.
5. Rein D, Wittenborn J, Zhang X, Song M, et al., Vision Cost-effectiveness Study Group. The potential cost-effectiveness of amblyopia screening programs. J Pediatr Opthalmol Strabismus. 2012; 49(3);146-155.
6. Holmes JM, Lazar EL, Melia BM, et al. Effect of age on response to amblyopia treatment in children. Arch Ophthalmol. Nov 2011;129(11):1451-7.
7. InfantSee website. www.infantsee.org. Accessed October 2015.
8. Amblyopia. www.aapos.org/terms/conditions/21. Updated 05/2015. Accessed 10/2015.
9. American Optometric Association official website. www.aoa.org. Updated November 2015. Accessed October 2015.

