Uncovering the underlying causes of band keratopathy (BK) is, by no means, a simple task, but it is something every optometrist is equipt to handle. The process requires a comprehensive approach to gathering the patient’s history and employing testing techniques. On top of that, the skilled clinician is responsible for deciding whether—and when—to treat. If the case calls for it, the OD can often treat noninvasively in an outpatient setting at the slit lamp.
This article provides a detailed look at each step of treating a BK patient, from presentation to surgical management.
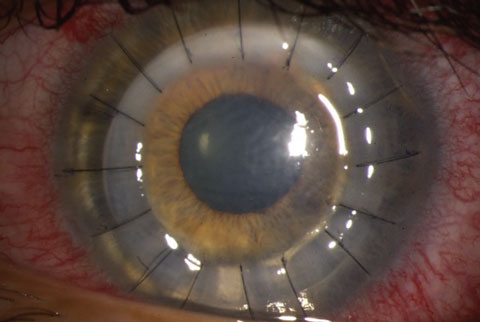
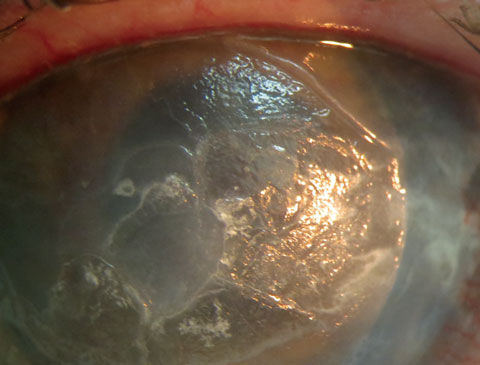 |
| This patient displays band keratopathy in a pre-phthisis non-seeing right eye. EDTA-assisted removal was initiated to resolve the non-healing central defect. Click image to enlarge. |
Presentation
Patients with band keratopathy may present for care with a variety of complaints. Cases of decreased vision, foreign body sensation, eye irritation, photophobia or concern about why their eye’s appearance has changed all have the potential to be BK.1 Early BK may go unnoticed by the patient and only become apparent upon routine slit lamp examination. In many cases, however, BK is associated with long-standing ocular disease, and the patient is fully aware of the condition.1
One study shows the most common causes of BK are chronic (28%) and idiopathic (26%) corneal edema.2
A thorough consideration of the differential diagnosis, possible causes and treatment options is essential. Clinicans must emphasize the risk of vision loss and treatment options, as patients who are asymptomatic may not consider cosmesis reason enough to undergo surgery.
BK is characterized by the appearance of an interpalpebral, horizontal, opaque grayish-white band across the central cornea. It is formed by the precipitation of calcium salts on Bowman’s layer, directly under the epithelium.1 The extreme periphery of the cornea may be spared because of the presence of limbal blood vessels exerting a buffering effect. Holes in the plaque are often present and are caused by corneal nerves crossing Bowman’s membrane to the epithelial surface. The band usually initiates in the periphery and progresses towards the center, but may, on occasion, begin centrally. Calcium deposits may be very fine or thick and plaque-like. Thick plaques have a tendency to partially flake off, especially in the periphery. This will cause epithelial defects and pain. In those patients with otherwise healthy eyes, visual acuities will decrease in proportion to the density of calcium salt deposition on the central cornea.
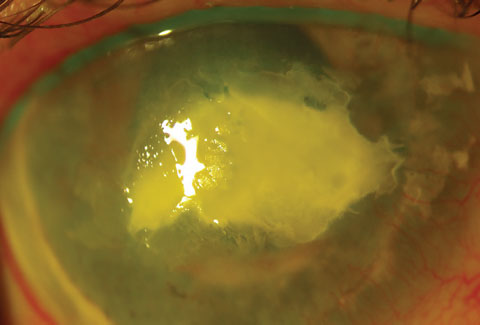 |
| This image shows the same eye as seen in the previous image, post procedure. Unfortunately, the eye became phthisical and had to be enucleated. Click image to enlarge. |
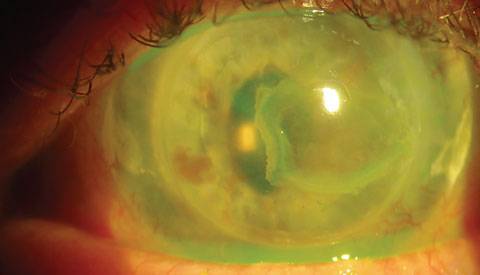 |
| Recurrence of BK in seeing left eye of same patient. This eye with ACIOL and penetrating keratoplasty for band keratopathy had recurrence despite efforts to address systemic causes (patient discontinued vitamin D). Click image to enlarge. |
Local Causes
The underlying cause of BK is abnormal levels of calcium and phosphate, which are both present at near their solubility limit in tears, aqueous humor and corneal tissue. Increased evaporation of tears promotes precipitation of these salts, especially in the interpalpebral area. Therefore, keratitis sicca is a significant risk factor for BK and should be ruled out as a cause. Even when calcium and phosphate levels are normal, elevation of the surface pH (alkalosis) favors precipitation. Alkalosis can be seen in chronically inflamed eyes and may explain the increased risk of BK in patients with chronic uveitis.3-5 Conditions such as juvenile idiopathic arthritis with uveitis, chronic herpes simplex and zoster keratitis, sarcoidosis, discoid lupus erythematosus and tuberous sclerosis are all associated with BK.3-5
Endothelial compromise and associated corneal edema may also result in calcium deposition and BK. This process is sometimes seen in aphakic patients who have silicone oil inside the eye, and seems to be due to the oil’s contact with the posterior cornea.6-8 One study concluded that BK was one of the main complications in 8% of patients treated with silicone oil in whom the oil remained in the eye for an average of 30 months, which is significantly longer than usual.6 The exact reasons for this association remain unclear.7,8
Ocular conditions that are associated with BK, but for which the mechanism is not clear, include end-stage glaucoma, corneal dystrophies and neurotrophic keratitis.9,10 It is possible that endothelial compromise plays a role in some of these conditions.
A number of topical medications can cause calcium precipitation and BK, including ophthalmic drops containing phosphates, such as steroid phosphates and other eye drops containing phosphate buffers.11 One study shows the risk for BK doubled when corneal alkali burns were treated with ophthalmic drops containing phosphate.12 Pilocarpine containing mercury-based preservatives was shown to increase the risk for BK as well.12 Mercury initiates changes in the corneal collagen that, in turn, causes deposition of calcium. Some surgical procedures that change the corneal surface or the endothelium increase the risk for BK, as does the use of some early viscoelastic preparations and, as mentioned, the intraocular presence of silicone oil and the intraocular use of tissue plasminogen activator.12
Finally, patients exposed to mercury vapor or calcium bichromate vapors, which can occur in certain industrial occupations, can develop BK.12
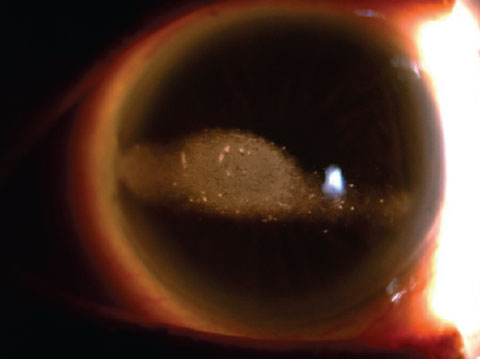 |
| This otherwise healthy eye clearly displays band keratopahty. |
Systemic Causes
Besides local causes of calcium and phosphate imbalance, elevated serum levels associated with systemic disease can tip the balance towards precipitation as well. Especially in patients who present with new-onset BK without any ocular risk factors, a systemic cause should be investigated. Systemic diseases correlated with BK usually are associated with hypercalcemia and include hyperparathyroidism, excessive vitamin D intake, endstage renal disease, hypophosphatasia, milk-alkali syndrome, Paget disease, sarcoidosis, discoid lupus erythematosus, gout (in the form of urate crystals), malignancy (such as iris melanoma) and tuberous sclerosis.13,14 Milk-alkali syndrome (also called calcium-alkali syndrome), caused by excessive intake of calcium carbonate usually for dyspepsia, is on the rise and is currently the third most common cause of patients admitted to the hospital for hypercalcemia.15 Hypophosphatasia is a rare inherited mutation in the enzyme alkaline phosphatase that leads to breakdown of bone and teeth. ODs must communicate effectively with the patient’s primary care provider to ensure that the appropriate systemic management is completed before initiating corneal treatment. The systemic control of hypercalcemia is complex and may require surgical intervention (such as with an overactive parathyroid gland) or medications that include calcimimetics, biphosphonates and prednisone (depending on the cause of the hypercalcemia). It may result in a medical emergency in the case of extremely high calcium levels, and may require rapid administration of IV fluids and diuretics to avoid heart arrhythmia and damage to the nervous system.16
Differential Diagnosis
A number of corneal conditions may present similarly to BK.17,18
Gout can be associated with corneal uric acid deposits similar in appearance to BK and is actually considered a form of BK by some. Gout is associated with joint pain, swelling and redness.
Interstitial keratitis can present in a similar fashion; however, deeper stromal scarring is expected.
Primary and secondary calcarous degeneration of the cornea, while grossly similar, can easily be distinguished at the slit lamp; as the calcium deposit is present within the stroma as well.19
Calciphylaxis, a condition of vascular calcification and skin necrosis, was once thought to be a hypersensitivity reaction to specific antigens, but is now thought to be multifactorial.20 It is more common in patients with endstage renal disease and generally associated with intensly painful, dark purple skin lesions. This is a potentially fatal disease.21
Spheroidal degeneration, also known as Labrador keratopathy, is usually associated with environments with intense chronic UV exposure. The corneal lesions may be more elevated and more yellow in appearance, and often interpalpebral conjunctival findings are found as well.
Ciprofloxacin (and also ofloxacin and norfloxacin) crystalline deposits may also be confused with BK. A detailed history should allow the practitioner to determine its cause. Discontinuation generally leads to resolution, while more extensive deposits may interfere with re-epithelialization.
Advanced basement membrane dystrophy or Salzmann nodular degeneration can cause subepithelial opacification that can grossly appear similar to BK. Unlike BK, it usually has a vascular component, and does not spare the limbus and does not present with clear islands within the lesion.
Familial BK is a rare disorder displaying an autosomal inheritance (both dominant and recessive inheritance has been reported) that the astute practitioner can uncover in the absence of local or systemic causes after doing a thorough pedigree analysis.22
 |
 |
| A patient pre- (top) and post- (bottom) EDTA assisted scraping of large calcific plaques. The goal with this patient was comfort, not visual rehabilitation. |
Systemic Considerations
For patients who present with BK in the absence of a known underlying cause, serum calcium and phosphate levels should be obtained along with renal function tests, such as blood urea nitrogen and creatinine. If sarcoid is suspected, either from ocular or systemic findings, angiotensin-converting enzyme testing, chest radiography, or chest spiral CT scanning should be obtained. In otherwise idiopathic cases, parathyroid hormone levels should be checked as well. If surgical treatment is decided by the OD and the patient, treat any underlying systemic or ocular condition first, as otherwise recurrence of BK is highly likely. Dietary modifications are indicated in patients with excessive vitamin D or milk-alkali syndrome.
Non-surgical Management
Many patients will present with BK caused by a history of ocular surgery, chronic inflammation or phthisis. These patients may not be symptomatic and may not benefit visually from surgical treatment. Exercise caution with patients who request surgical treatment solely for cosmetic reasons, as eyes with BK often have other conditions and may not heal as well.2
When such a patient presents with symptoms, a non-surgical alternative treatment may include the fitting of a bandage contact lens. Antimicrobial topical therapy should be initiated to reduce the risk of infection in overnight contact lens wear on a compromised cornea. Prosthetic opaque contact lenses can also be fit for cosmetic concerns. Lubrication in the form of artificial tears, gels and ophthalmic ointments may help significantly in patients who present with foreign body sensation, tearing and photophobia and should be first-line treatment. The application of an amniotic membrane device has also been shown to promote healing of BK.1
Surgical Management
Once systemic and ocular causes of BK are eliminated and/or treated, and after risks and benefits are discussed with the patient, promptly offering surgical treatment will benefit your patients. One study showed that the majority of patients experienced partial or complete symptomatic relief (98%) while one third of patients improved two lines at two months and 36 months.2
Treatment is relatively straightforward and can even be done at the slit lamp. It always requires removal of the corneal epithelium, followed by superficial debridement (corneal scraping) in the presence of ethylenediaminetetraacetic acid (EDTA).23,24 In some cases, when the surface is still irregular after the calcium is removed, excimer laser is used to smooth the corneal surface, but this will result in some refractive change.25
Patients need to be informed of possible adverse outcomes, including corneal scarring and vision loss, but the incidence of such complications has been reported as close to zero.24
Procedure
Removal of calcium is preferably performed under the operating microscope by chelation using a 3% EDTA solution but can be done at the slit lamp if needed. The procedure’s steps are:17
1. Anesthetize the eye with a topical anesthetic (e.g., proparacaine) and place an eyelid speculum.
2. Debride the corneal epithelium. This can be done with a sterile Beaver blade or an Amoils scrubber.
3. The 3% EDTA solution is then applied to the area of band keratopathy. This is typically done by using a corneal shield/filter paper disc, cut strips of Weck-Cel or sterile cotton tip applicators soaked with EDTA. Alternatively, a reservoir such as a LASIK well can be placed over the cornea and filled with EDTA. The EDTA is applied in three-minute intervals, alternating with thorough irrigation with balanced salt solution. This is done until the calcium clears, which may take 10 to 60 minutes. Care should be taken to avoid toxicity to limbal cells and minimize irritation of the conjunctiva. Thin calcium deposits may come off in five minutes, while thick plaques may take 30 to 45 minutes to dissolve.
Completing the procedure at the slit lamp allows for better visualization. However, when the procedure is performed in upright position, the drainage of EDTA into the inferior fornix increases the risk of a conjunctival chemical burn. Placing sponges containing EDTA on the cornea is much easier in a reclined position as well.
The main advantage of using the EDTA is to minimize damage to Bowman’s layer and reduce the risk of an irregular refractive surface that may result from aggressive debridement with a blade. Gentle scraping in between EDTA applications can be performed and may help speed the process.
5. If the corneal surface is extremely irregular after the procedure, polishing the Bowman’s layer with a 5mm diamond burr or phototherapeutic keratectomy can smooth the surface. Of note, if any residual calcium is left over, excimer laser treatment will cause worsening of the corneal irregularity, as the laser preferentially ablates the calcium.25 Alternatively, a gas permeable contact lens can be used afterwards.
6. A soft contact lens is typically placed at the end of the procedure and prophylactic topical antibiotics are used until the epithelial defect has healed. We frequently prescribe topical steroids to modulate healing and reduce scarring. We occasionally use a sutureless amniotic membrane to enhance healing, particularly when delayed epithelialization is anticipated, such as in patients with neurotrophic disease, chronic ocular surface inflammation or advanced age. These cases may be reserved for a specialist since a non-healing epithelial defect may ensue and must be treated aggressivly.
More advanced cases, particularly those that invade Bowman’s membrane, may require a more extensive lamellar keratectomy technique such as deep anterior lamellar keratoplasty (DALK).26
Extensive keratectomy may cause bleeding from the limbal vessels, particularly in cases associated with superficial corneal neovascularization or interstitial keratitis. This can be controlled with pressure or topical vasoconstrictors, and cautery should be avoided to prevent damage to the limbal stem cells.
 |
| A patient’s left eye following a DALK procedure. |
Postoperative Care
The patient should be examined five to seven days following surgery. Examination of the epithelium under the contact lens can be performed with fluorescein. Steroids are tapered and the contact lens and antibiotic drops are discontinued once the epithelial defect heals.
Residual anterior stromal scarring may be amenable to excimer laser PTK to improve vision. PTK may also be used to improve the ocular surface and prevent recurrent erosions.
The patient should be checked every three to 12 months, depending on the severity of symptoms. Surgical removal can be repeated if the band keratopathy recurs.
Complications
The main complications related to the removal of calcium deposits on the corneal surface include pain, corneal scarring, corneal edema, infection, decreased vision, non-healing epithelial defect and increased irregular astigmatism. EDTA is toxic to the ocular surface, and inadequate removal during or after the procedure will cause a chemical burn. Recurrence is common, and repeated treatments may be needed. Recurrence is most common in cases of uveitis-induced BK.1,2
Occasionally, a mild subepithelial haze can be seen weeks after EDTA chelation, which may resolve on its own. A mild topical steroid (e.g., fluorometholone 0.1%) may help to resolve this haze. If there is significant damage to the Bowman’s membrane, the haze may be permanent.
Significant BK is a disease that can and should be treated by EDTA-assisted surgical removal. BK in otherwise healthy patients should be evaluated for systemic causes, including hypercalcemia. Treatment considerations include the likelihood of visual recovery, the presence of pain, photophobia and foreign body sensation and concern for cosmesis.
The overall health of the eye and its ability to heal after the treatment should also be considered. When surgical treatment is not an option, active lubrication or the use of a bandage or prosthetic contact lens are options as well.
Dr. Stokkermans is the director of Optometric Services and Dr. Gupta is the director of Cornea and External Diseases at University Hospitals Cleveland Medical Center. Drs. Stokkermans, Gupta and Sayegh are attending faculty at Case Western Reserve University and provide a team approach for the treatment of corneal disease.
|
1. Jhanji V, Rapuano C, Vajpayee R. Corneal calcific band keratopathy. Curr Opin Ophthalmol. 2011 Jul;22(4):283-9. 2. Najjar D, Cohen E, Rapuano C, Laibson P. EDTA chelation for calcific band keratopathy: results and long-term follow-up Am J Ophthalmol. 2004 Jun;137(6):1056-64. 3. Bernauer W, Thiel M, Kurrer M, et al. Corneal calcification following intensified treatment with sodium hyaluronate artificial tears. Br J Ophthalmol. 2006 Mar;90(3):285-8. 4. Doostdar N, Manrique C, Hamill M, Barron A. Synthesis of calcium-silica composites: a route toward an in vitro model system for calcific band keratopathy precipitates. J Biomed Mater Res A. 2011 Nov;99(2):173-83. 5. Daniel E, Pistilli M, Pujari S, et al. Risk of hypotony in noninfectious uveitis. Ophthalmology. 2012 Nov;119(11):2377-85. 6. Morphis G, Irigoyen C, Eleuteri A, et al. Retrospective review of 50 eyes with long-term silicone oil tamponade for more than 12 months. Graefes Arch Clin Exp Ophthalmol. 2012 May;250(5):645-52. 7. Sternberg P, Hatchell D, Foulks G, et al. The effect of silicone oil on the cornea. Arch Ophthalmol. 1985 Jan;103(1):90-4. 8. Federman J, Schubert H. Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery. Ophthalmology. 1988 Jul;95(7):870-6. 9. Kennedy R, Roca P, Landers P. Atypical band keratopathy in glaucomatous patients. Am J Ophthalmol. 1971 Nov;72(5):917-22. 10. Lam H, Wiggs J, Jurkunas U. Unusual presentation of presumed posterior polymorphous dystrophy associated with iris heterochromia, band keratopathy, and keratoconus. Cornea. 2010 Oct;29(10):1180-5. 11. Taravella M, Stulting R, Mader T, et al. Calcific band keratopathy associated with the use of topical steroid-phosphate preparations. Arch Ophthalmol. 1994 May;112(5):608-13. 12. Kompa S, Redbrake C, Dunkel B, et al. Corneal calcification after chemical eye burns caused by eye drops containing phosphate buffer. Burns. 2006 Sep;32(6):744-7. 13. Porter R, Crombie A. Corneal and conjunctival calcification in chronic renal failure. Br J Ophthalmol. 1973 May;57(5):339-43. 14. Shah P, Shields C, Shields J, Di Marco C. Band keratopathy secondary to an iris melanoma. Cornea. 1991;10(1):67-9. 15. Patel A, Goldfarb S. Got calcium? Welcome to the calcium-alkali syndrome. J Am Soc Nephrol. 2010;21(9):1440-3. 16. Mayo Clinic Staff. Diseases and Conditions: Hypercalcemia. Avaliable at www.mayoclinic.org/diseases-conditions/hypercalcemia/basics/treatment/con-20031513. Accessed December 9, 2016. 17. Gerstenblith A, Rabinowitz M. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 6th Ed. Philadelphia: Lippincott Williams & Wilkins; 2012. 18. Roy FH. Corneal and conjunctival calcification. In: Roy FH, Fraunfelder FW, Fraunfelder FT.Roy and Fraunfelder’s Current Ocular Therapy. 6th ed. Current Therapy series. Philadelphia: Elsevier/Saunders;2008:337–8. 19. Lavid F, Herreras J, Calonge M, et al. Calcareous corneal degeneration: report of two cases. Cornea. 1995 Jan;14(1):97-102. 20. Wolff K, Johnson R, Saavedra A. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 7th ed. McGraw Hill: 429. 21. Angelis M, Wong L, Wong L, Myers S. Calciphylaxis in patients on hemodialysis: A prevalence study. Surgery. 1997;122:1083–90. 22. Arora R, Shroff D, Kapoor S, et al. Familial calcific band-shaped keratopathy: report of two new cases with early recurrence. Indian J Ophthalmol. 2007 Jan-Feb;55(1):55-7. 23. Najjar D, Cohen E, Rapuano C, Laibson P. EDTA chelation for calcific band keratopathy: results and long-term follow-up. Am J Ophthalmol. 2004 Jun;137(6):1056-64. 24. Im S, Lee K, Yoon K. Combined ethylenediaminetetraacetic acid chelation, phototherapeutic keratectomy and amniotic membrane transplantation for treatment of band keratopathy. Korean J Ophthalmol. 2010 April;24(2):73–7. 25. Sharma N, Mannan R, Sinha R, et al. Excimer laser phototherapeutic keratectomy for the treatment of silicone oil-induced band-shaped keratopathy. Eye Contact Lens. 2011 Sep;37(5):282-5. 26. Wee S, Choi S, Kim J. Deep anterior lamellar keratoplasty using irradiated acellular cornea with amniotic membrane transplantation for intractable ocular surface diseases. Korean J Ophthalmol. 2015 Apr;29(2):79-85. |

