Keen intellects have been trying to tackle the problem of presbyopia at least since the time of Benjamin Franklin, who wrote in 1784 that he was “happy in the invention of double spectacles, which serving for distant objects as well as near ones, make my eyes as useful to me as ever they were.” Many people today remain just as happy with modern descendants of that same approach, but that hasn’t stopped researchers from continuing to explore innovative approaches, so that the billions of presbyopes in the world can each find a solution that suits them. Here is a look at the latest emerging options to address this all-but-inevitable human need.
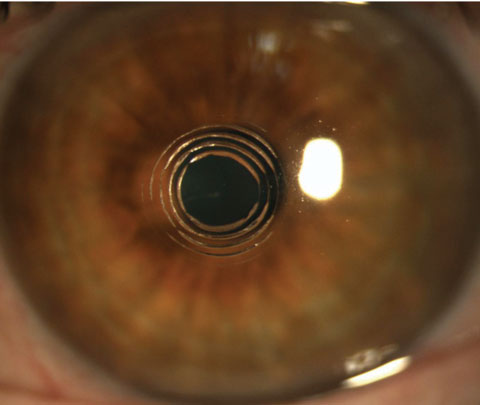 |
| Clinical view of intrastromal incisions three hours post-Intracor treatment. Photo: Technolas Perfect Vision. |
Contact Lenses
Data suggests the majority of contact lens wearers prefer to stay in contacts once they become presbyopes; in fact, 91% of contact lens wearers ages 35 to 55 hope to continue wearing contact lenses.1 “Many presbyopes are interested in occasional contact lens wear, for which daily disposable lenses are an ideal option,” says Thomas G. Quinn, OD, of Drs. Quinn, Foster and Associates in Athens, Ohio.
The advent of stable lens platforms such as hybrid and scleral lenses is also good news for presbyopes with corneal astigmatism, adds Clark Chang, OD, director of the specialty contact lens service at the Cornea and Laser Eye Institute in Teaneck, NJ. He explains that aspheric optics and reverse geometry in hybrid multifocal lenses allow for an extended range of functional vision, while the ultra-stable nature of scleral lenses provides options for patients with residual cylinder through the concurrent provision of multifocal optics with front toric corrections.
Today’s soft disposable multifocals also provide better day-to-day comfort— important in this population, as presbyopes often exhibit drier eyes—while high Dk lens materials combined with plasma treatment make modern hybrid and scleral lenses more ocular surface-friendly than older generations. They may reduce patient dropout due to discomfort even during allergy season, Dr. Chang says, while the new aspheric multifocal hybrids and toric scleral lenses offer a more continuous range of vision than ever before. New lenses in the pipeline to supplement your arsenal include:
Choosing the Right Presbyopia Correction “Communication is everything,” says Dr. Freeman. “The eye care provider involved with a patient’s care must listen to a patient’s goals and expectations of treatment, whether it’s glasses or contact lenses, or some type of vision correction surgery,” he says. If surgery is the decided course, the patient and provider need to be on the same page regarding the expected outcome of any surgery, says J. Christopher Freeman, OD. “After a patient’s goals and expectations are made known, the providers need to let the patient know what can be delivered. Visual demands, goals for improvement in certain lifestyle or leisure activities, as well as physical and ocular health are a few of the important considerations that should be addressed when developing a treatment plan. If the anticipated outcome is not congruent with the goal, then the patient’s goal may need to be adjusted and the expectations reset.” Success is much more likely with this approach, Dr. Freeman says. For Dr. Chang, a thorough understanding of patients’ lifestyle and visual habits is essential to guide the decision-making process. For presbyopia patients who are not yet suitable for IOL discussions (i.e., ages 40 to 60), contact lenses and the Kamra inlay can be effective management options for typical day-to-day tasks. If a patient has high demand for near acuity, bifocal GP lenses may still be one of the best options. For those patients who have sufficient crystalline lens change and whose best contact lens corrected vision has been on the decline, then discussing a premium IOL is an excellent option, Dr. Chang says. |
• Bausch + Lomb’s Ultra for Presbyopia. Expected to arrive in the second quarter of 2016, this monthly replacement silicone hydrogel lens will combine the three-zone progressive design from the company’s Biotrue OneDay multifocal with its Ultra contact lens material. The lens contains polyvinyl-pyrrolidone, which Bausch + Lomb says enhances wettability to aid in providing better all-day comfort; the lens has the highest Dk/t (163) and lowest modulus (70) among the silicone hydrogels, according to B+L. Its aspheric optics provide good vision even in low light, and the three-zone design allows for smoother transitions as the patient shifts gaze, the company says.
• Brien Holden Vision’s extended depth of focus (EDOF) contact lenses. These recently received FDA clearance and are scheduled to be available this year. The design uses higher-order aberrations to improve image quality over a wide range of distances while minimizing ghosting and haloes and should perform relatively independent of a patient’s natural aberrations and variation in pupil size, the company says.
• E-Vision Smart Optics electronic contact lens. This device will retain the look and feel of conventional lens, but adds a layer of liquid crystal material that can be “tuned” to different focal lengths via embedded electrodes, allowing the wearer to change prescription in as little as 200 milliseconds, the company says. The first prototype will be available by late 2016, says E-Vision.
• Google and Alcon’s ‘smart’ lenses. The two companies are partnering to develop a lens that incorporates embedded sensors, microchips and other miniaturized electronics. Alcon expects the lens to provide accommodative vision correction to help restore the eye’s natural autofocus on near objects in the form of an accommodative contact lens or intraocular lens (IOL)implanted during refractive cataract treatment.
“The ‘smart’ lens design offers some promise to be a game changer —if it delivers,” suggests Dr. Quinn. “I can’t wait to get my hands on it.”
Until then, conventional multi-focal contact lenses continue to improve with each new generation, and 2016 looks to be a year marked by progress.
Multifocal and Accommodating IOLs: The New Generation
Currently, there are four predominant surgical solutions for presbyopia—multifocal IOLs, monovision, accommodating IOLs and extended depth of focus IOLs—that incorporate intraocular lenses after cataract surgery, says Eric Donnenfeld, MD, clinical professor of ophthalmology at NYU and past president of the American Society of Cataract and Refractive Surgery. Monovision and multifocal lenses have been around for a long time, he notes, but “what is most exciting are the new, lower-add multifocal lenses that reduce the size of haloes and are actually much better tolerated than the older generation of four diopter lenses.”
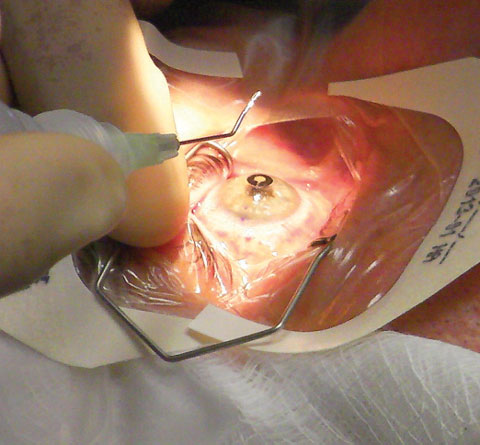 |
| Intraoperative photo of a patient undergoing Kamra inlay implantation. Photo: Clark Chang, OD. |
Two of the newest additions are the AcrySof IQ Restor +2.5D IOL (Alcon) and the Tecnis Multifocal +2.75D and +3.25D (Abbott Medical Optics). The FDA approved the former, which uses fewer diffractive zones and a larger central refractive zone than other IOLs for better distance vision, in April 2015.2 Alcon says it’s ideal for patients with “distant-dominant lifestyles.” Dr. Donnenfeld notes that a toric version of this intraocular lens should be released shortly.
The one-piece Tecnis multifocal IOL +2.75D improves long intermediate acuity (~50cm theoretical reading distance) while the +3.25D lens improves close intermediate viewing (~42cm distance), AMO says.
Also on the multifocal IOL horizon are three tri-focal lenses currently available in Europe: AcrySof IQ PanOptix trifocal (Alcon), PhysIOL (FineVision) and Lisa Tri 839MP (Carl Zeiss Meditec). While still not available in the United States, Dr. Donnenfeld believes these advancements look promising as future treatment options.
The only FDA-approved accommodative IOL currently available remains the tried and true Crystalens (Bausch + Lomb) and its toric version, Trulign. However, other promising designs are making their way through the pipeline:
• Tetraflex (Lenstec). This flexible, non-hinged, single-optic IOL features closed-loop haptics angled anteriorly 10°, causing the optic to flex and change curvature with accommodation. A study of functional vision showed improved ability to read 80 words per minute or more at print sizes as small as 20/25 with the Tetraflex.3
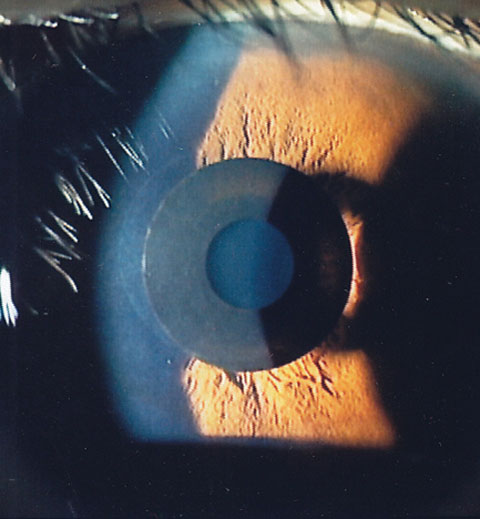 |
| Slit lamp view of the Kamra inlay in position. Photo: Minoru Tomita, MD. |
• FluidVision Lens (Power Vision). This IOL is an acrylic implant filled with silicone oil that changes curvature with accommodation. As the ciliary muscle contracts and relaxes, energy is transferred to the zonules and lens capsule, where it squeezes fluid from the haptics into the optic to increase its anterior curvature.
• Sapphire AutoFocal IOL (Elenza). Electroactive optics in this intraocular lens help it change power when accommodation is necessary. A microscopic battery stimulates internal liquid crystals when pupil size decreases.
• AMO Tecnis Symfony. This extended-depth-of-focus lens takes a different approach to extending a patient’s range of vision by addressing the optical property known as chromatic aberration.4 Dr. Donnenfeld, who was part of the investigative team in an FDA trial of the lens, explains that most subjects tolerated the Tecnis with minimal distance distortion, as well as reduced glare and halo. “You do lose a little bit of contrast, but it’s [part of] a whole new generation of lenses that appear to be very interesting,” he says, adding that the device is likely to be available in the United States in 2017.
• Calhoun Vision Light Adjustable Lens. This IOL’s power is adjusted after the lens is in place by irradiating the lens’s special silicone material with ultraviolet light, which changes the lens’s shape and therefore its power.4 A Phase III study is underway.
• AkkoLens Lumina. The Lumina is a dual-optic lens that relies on the action of the ciliary body for its effect.4 The company anticipates receiving the CE mark for the Lumina, and it plans to expand clinical trials in other countries.
• Vision Solutions Technologies’ LiquiLens. Created by optometrist Alan Glazier, this bi-fluidic IOL has a gravity-based mechanism that shifts the focal plane on downgaze by altering interplay of fluids against one another.4
Ophthalmic Lenses: Still Making Strides “Spectacle lens technology continues to advance from early progressive addition lenses to today’s ‘free form’ lenses, also known as digital lenses,” says Dr. Freeman. These lenses provide an array of computer-calculated, customizable parameters to best suit a given patient’s prescription, visual demands and desired frame, he says. “For example, with advanced computer algorithms, a corridor length can be designed to custom fit a patient’s frame of choice, along with the appropriate width of distance or near vision portion of the lens, and can even be optimized to the fitted frame’s pantoscopic tilt and face-form wrap. These personalized progressive addition lenses can reduce unwanted distortions, improve adaptation and ultimately increase patient satisfaction,” Dr. Freeman says. Many of the new digital lenses now offer technologies that the companies say will eliminate eye fatigue and boost reading on digital devices. This new era of progressives includes Essilor’s Varlilux portfolio, which has incorporated technologies that provide sharper vision in all lighting condition, easier transitions between distance and near zones, and a reduction of swim, according to the company. Other digital lenses include the Shamir’s Autograph, inTouch, Spectrum, Element, FirstPal, Creation and Piccolo; Hoya’s Lifestyle 2, Mystyle and Summit iQ; and Zeiss’ Precision Portfolio and Individual 2. Also from Zeiss is the high-definition Sola HDV. Yet another high-definition lens is the Seiko Supercede from Seiko Optical Products of America. |
• AcuFocus IC-8. This combination device consists of a small-aperture “mask” and an acrylic IOL lens platform, Dr. Chang says. “The acrylic platform is similar to the other foldable IOLs in use today, so no new surgical delivery technique will be required,” he says. The opaque mask component in the center of the IOL optic has an outer diameter of 3.23mm and an inner aperture measuring 1.36mm in size to offer similar benefit of extended depth of focus as in a Kamra inlay (discussed below), he adds. This IC-8 IOL received CE mark in the fall of 2014.
Inlays: The Latest Frontier
A relatively new approach to presbyopia correction, corneal inlays improve near vision without hindering distance vision in emmetropic presbyopes.
“Corneal inlays serve an exciting niche market for the emmetropic presbyope looking to restore the lifetime of excellent vision that seems to have been stolen from them,” says J. Christopher Freeman, OD, of the Landstuhl Regional Medical Center Department of Ophthalmology in Landstuhl, Germany.
In April 2015, the FDA approved the Kamra inlay (AcuFocus) to improve near vision in certain patients with presbyopia. This thin (5µm), small (3.8mm) disc has a 1.6mm central opening that acts like a pinhole to increase the patient’s depth of field and improve near vision with little effect on distance vision. Thousands of micro-perforations in the donut-shaped Kamra inlay allow nutrients to pass through the implant within the cornea, Dr. Freeman says.
The “pseudo-random” distribution pattern of the perforations also ensures the delivery of more focusable light rays to the retinal plane, says Dr. Chang. This allows for better optical regulations by the Kamra inlay and improves visual function in dimmer environments compared to previous generations of small aperture inlays, Dr. Chang says.
“What’s nice about the Kamra inlay is that it doesn’t distort vision,” Dr. Donnenfeld explains. “There is no change in refractive index of the cornea, and as with all the inlays, I don’t say it’s reversible, but removable.”
Vance Thompson, MD, of Sioux Falls, SD, who was part of the scientific team in the FDA Kamra inlay clinical trials, says results of the study found, on average, near vision improved from a pre-op Jaeger score of J8 to J2 post-op. “The vast majority [of patients] maintained their uncorrected distance vision at 20/20 or 20/25,” he says. “Normally to get that sort of near improvement with monovision, we would have to sacrifice distance much more, so we were amazed at the improvement in near and how distance was preserved.”
Dr. Thompson says he was surprised that intermediate vision was maintained or improved following the implantation of the Kamra inlay. This isn’t the case with monovision, where more near correction hurts intermediate vision. Also unlike monovision, the overall results post-op didn’t lessen with time. “This is very exciting technology for my presbyopic patients with clear lenses,” Dr. Thompson says.
Furthermore, adds Dr. Quinn, the procedure itself is relatively quick and leads to minimal patient discomfort. “It saves the patient from the inconvenience of lens application and removal required by contact lens wear.” However, “there are some reports of increase glare at night. Challenges with viewing the retina during retinal surgery have been reported when the inlay is in place,” Dr. Quinn says.
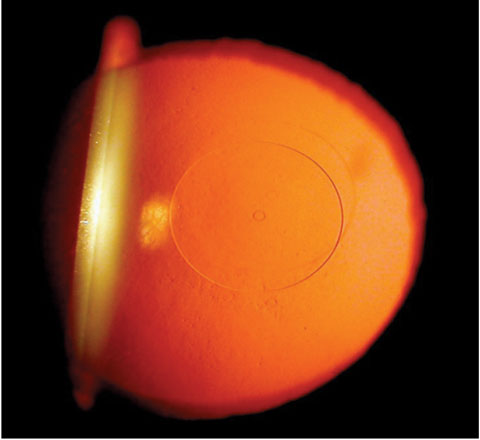 |
| Flexivue Microlens, within which a 0.5mm central perforation can be seen with retroillumination. Photo: Clark Chang, OD. |
A few other inlays are moving through the approval process and may be available in the near future:
• The Raindrop (ReVision Optics). This hydrogel plastic inlay typically is placed within the cornea of the non-dominant eye under a LASIK-style flap created using a femtosecond laser. When in position, it changes the curvature of the cornea so the front of the eye acts like a multifocal contact lens. In November 2015, the FDA accepted the company’s premarket approval submission; the product could reach the US by 2017. Dr. Donnenfeld notes patients may sacrifice some quality of distance vision, but overall the loss is minimal.
• Flexivue Microlens (Presbia). Also pending FDA clearance, this hydrophilic acrylic inlay measures 3.2mm in diameter and 0.015mm/15µ in edge thickness, is offered in powers ranging from +1.5D to +3.5D, in 0.25D increments and implanted in the non-dominant eye. Presbia completed its second stage enrollment of its FDA pivotal study in September 2015. A recent study found that 12 months after implantation, the inlay seems to be an effective method for the corneal compensation of presbyopia in emmetropic presbyopes between the ages of 45 and 60.5
• Icolens (Neoptics). Still in the early stages of development, this hydrophilic copolymer inlay has a diameter of 3.0mm and an edge thickness less than 15µ (depending on refraction). For presbyopia, it offers power ranging from +1.5D to +3.0D (in 0.5D steps).
“Based on my current knowledge of available inlays, I think there may be overlapping clinical indications for each,” Perry Binder, MD, writes in a recent issue of EuroTimes. “This can only benefit patients’ needs. Until we develop a safe and predictable means of replacing the aging dysfunctional lens with a biocompatible intracapsular polymer, the intracorneal inlay in its current iteration and possibly newer alloplastic materials will offer the most predictable, easily removable and safe refractive surgical correction of presbyopia.”
Other Surgical Techniques
Inlays and new IOLs aren’t the only surgical innovations to pique researchers’ interests, however:
• Presby-LASIK. This is an aspheric modification of the cornea under a flap using an excimer laser that creates a multifocal cornea by inducing higher-order aberrations that increase depth of focus.6
Central presby-LASIK creates a steeper myopic corneal center surrounded by a flat hyperopic periphery, inducing a negative spherical aberration.6 The pupil constricts with convergence, creating a pinhole effect.6 Peripheral presby-LASIK induces positive spherical aberration, which increases pseudo-accommodation. The flattened corneal center focuses distance, while the steepened periphery focuses near.6 Clinical outcomes for both peripheral and central presby-LASIK show promise, but further studies are needed to investigate long-term stability of the procedure and quality of vision under low contrast settings.7
Presby-LASIK has been around for a long time in other countries and is especially popular in South America, Dr. Donnenfeld says. However, there are no current active trials in the United States.
• Intracor. This procedure uses a femtosecond laser to create concentric, intrastromal cylindrical incisions that change the corneal biomechanics to reshape the cornea. Because the procedure is intrastromal, there is no incision of the epithelium, endothelium or Bowman’s or Descemet’s membrane. The internal rings created by the laser steepen the curvature of a small central zone in the cornea, which increases near vision. The FDA has not yet cleared Intracor for use in the United States, but the presbyopia correction treatment has shown promising results in early studies.8,9
• Scleral implants. While found to be ineffective in the past, these are back under the microscope, Dr. Donnenfeld says. A newer version of one such device, the VisAbility scleral implant (Refocus Group), uses four small implants placed in scleral tunnels 4mm posterior to the limbus, which the company says restores tension of the posterior zonules, giving the ciliary muscles more efficiency in reshaping the lens in presbyopic patients.10 Results of a recently completed FDA clinical trial were promising, with 96% of patients seeing J3, 20/40 or better uncorrected at near monocularly. All were better still binocularly.10
The concept of scleral expansion to tighten the zonules, increasing their ability to change crystalline lens shape, has been explored for over a decade, Dr. Quinn adds. One caveat, though, is that “tissue barriers are inserted into channels that maintain the scleral expansion. This is somewhat controversial, and the American Academy of Ophthalmology has stated clinical results with scleral expansion ‘have been disappointing’ and ‘leave little support’ for it as ‘an effective means of presbyopia correction,’” Dr. Quinn says.
• LaserAce system (Ace Vision Group). This developing technology uses an erbium-YAG laser to create numerous ablation spots through 90% of the scleral depth in an attempt to ease contraction of the ciliary muscle, the company says.
Correction by the Drop
Could your presbyopes one day be able to correct their vision by simply using an eye drop? A few research teams are currently working on this alternative treatment that also creates the pinhole effect as the inlays do, but noninvasively.
• Carbachol/brimonidine. Last year, researchers in Egypt conducted a double-masked, randomized placebo-controlled clinical trial with 48 naturally emmetropic and presbyopic subjects to investigate the use of a parasympathomimetic drug (carbachol) and an alpha-agonist (brimonidine) to treat presbyopia.11 “The monocular pharmacologic treatment of presbyopia with one drop a day of carbachol and brimonidine in the non-dominant eye permits acceptable reading vision for many presbyopes, even in older subjects,” says lead investigator Almamoun Abdelkader, MD, PhD. “Because of increased depth of focus from the smaller pupil, it does not blur distance or intermediate vision, as does typical monovision therapy, and the perception of normal brightness in the untreated eye eliminates symptoms of dimming from the smaller pupil of the treated eye.”
• Liquid Vision (Presbyopia Therapies). This drop is in Phase II clinical trials as a topical, reversible, short-term treatment for presbyopia. The investigational drug induces a miotic effect on the pupil that lasts approximately eight hours after instillation, developers say.12 By constricting the pupil and creating a pinhole effect, the drops help to improve near vision performance.
• PresbV Tears. Columbian researcher Felipe Vejarano, MD, is leading the investigation of this eye drop for presbyopia correction. Effects of the drop last four to five hours after application and result in increased near vision by three lines without diminished distance vision, Dr. Vejarano says. In some cases, the treatment may improve distance vision by one line, Dr. Vejarano said at the 2015 Academy of Ophthalmology meeting. The drop is applied to both eyes and, because of its pseudo-accommodation, can also improve night vision, he claimed.
Although eye drops can simulate the visual effect of a small-aperture inlay, miotics have a risk of retinal detachment, Dr. Binder notes in EuroTimes. “The effect of such drops lasts four to six hours, maximum, and takes time to develop,” he writes. “Patients desire instant near acuity and do not wish to wait 15 to 30 minutes before they can read. Having to take frequent drops is not much better than wearing reading glasses.” However, the impact of such a topical eye drop on non-small aperture inlays has the potential to enhance their outcomes, he adds.
Dr. Freeman says he is excited that new technology in presbyopia correction is advancing so quickly, and with it, an increase in the options to customize patients’ treatments. “Now we are able to address presbyopia with real solutions, and ever-improving ones, to help patients achieve their visual goals.”
“Presbyopia is a universal problem that is extremely debilitating to many patients older than 40, and we continue to seek solutions for this,” Dr. Donnenfeld says. The optimal solution is “going to be a true accommodating IOL that has no loss of contrast sensitivity,” he believes. “They will come eventually.”
|
1. Reindel WT, Edmunds FR. A clinical assessment of presbyopic soft contact lens designs: comparing the impact of SofLens multifocal contact lenses and Acuvue bifocal contact lenses on successfully adapted monovision patients. Review of Optometry. 2003 Apr 15;140(4). 2. Saxena V. Alcon intraocular lens gets FDA’s stringent PMA approval. Fierce Medical Devices. 2015 Apr 17. Available at www.fiercemedicaldevices.com/story/alcon-intraocular-lens-gets-fdas-stringent-pma-approval/2015-04-17. 3. Bohorquez V, Alarcon R. Long-term reading performance in patients with bilateral dual-optic accommodating intraocular lenses. J Cataract Refract Surg. 2010;36:1880-6. 4. Bethke W. IOL alternatives to multifocality, Review of Ophthalmology. 2015;22(1):32-8. 5. Limnopoulou AN, Bouzoukis DI, Kymionis GD, et al. Visual outcomes and safety of a refractive corneal inlay for presbyopia using femtosecond laser. J Refract Surg. 2013;29:12-8. 6. Crabb A, Krueger, R. The final cut: surgical correction of presbyopia. Review of Cornea and Contact Lenses. 2014 Nov;151(8):20-6. 7. Waring GO, Berry DE. Advances in the surgical correction of presbyopia. International Ophthalmology Clinics. 2013;53:129-152. 8. Khoramnia R, Fitting A, Rabsilber TM, et al. Intrastromal femtosecond laser surgical compensation of presbyopia with six intrastromal ring cuts: 3-year results. Br J Ophthalmol. 2015 Feb;99(2):170-6. 9. Thomas BC, Fitting A, Auffarth GU, et al. Femtosesecond laser correction of presbyopia (INTRACOR) in emmetropes using modified pattern. J Refract Surg. 2012 Dec;28(12):872-8. 10. Stephenson M. The future of presbyopia correction. Review of Ophthalmology. 2015 Feb;22(2):47-9, 71. 11. Abdelkader A. Improved presbyopic vision with miotics. Eye & Contact Lens. 2015 Sept;41(5):323-7. 12. Review of Cornea and Contact Lenses, June 15, 2014. Available at www.reviewofcontactlenses.com/content/c/48838. |

