 |
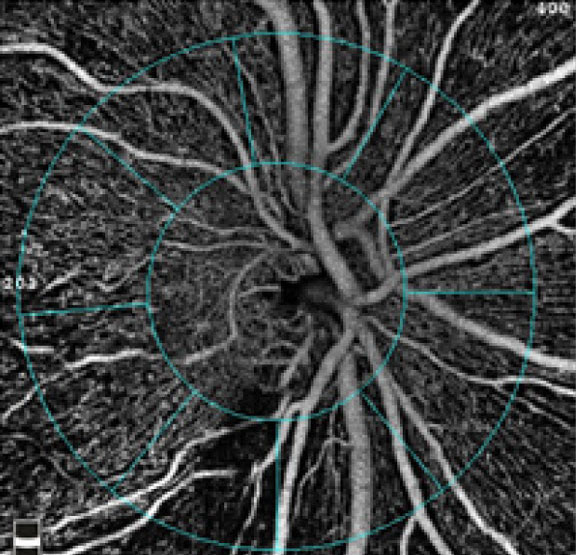
3D retinal imaging was actually shown to surpass the performance of RNFL thickness as a tool for glaucoma detection. Photo: Julie Rodman, OD. Click image to enlarge. |
Research continues to show that the retinal vasculature is fertile ground for new biomarkers that could help doctors understand and anticipate glaucoma’s course. Although OCT-A provides a wealth of information for glaucoma diagnosis, it does not delineate large vessels properly in 3D because it cannot visualize vertical vessels and is more targeted at capillaries in a 2D plane. The central retinal vessel trunk and its branches experience significant structural changes during the development and progression of glaucoma, which could accelerate further damage.
A study recently found that the 3D structural configuration of the central retinal vessel trunk could be used as a biomarker for glaucoma diagnosis. Its diagnostic power was found to outperform the gold-standard diagnosis parameter: RNFL thickness.
The researchers trained a deep learning network to automatically segment the central retinal vessel trunk and its branches from the B-scans of the OCT volume of the optic nerve head. A total of 4,108 participants (1,639 glaucoma and 2,469 non-glaucoma) were recruited for this study at three different sites. Those with an IOP of less than 21mm Hg, healthy optic discs with a vertical cup-to-disc ratio (CDR) less than or equal to 0.5 and normal visual fields tests were considered non-glaucoma cases, whereas subjects with glaucomatous optic neuropathy, vertical CDR >0.5 and/or neuroretinal rim narrowing with corresponding repeatable glaucomatous visual field defects were deemed glaucomatous.
The study then used two different approaches for glaucoma diagnosis. In the first, only 3D convolutional neural networks (CNNs) and the 3D structure of the central retinal vessel trunk and its branches provided the diagnosis. For the second approach, the team projected the 3D structure of the central retinal vessel trunk and its branches orthographically onto sagittal, frontal and transverse planes to obtain three 2D images, and then a 2D CNN was used for diagnosis. The diagnostic performance of the central retinal vessel trunk and its branches analysis was also compared with that of RNFL thickness (calculated in the same cohorts).
The 3D and 2D diagnostic networks were able to differentiate glaucoma from non-glaucoma subjects with accuracies of 82.7% and 83.3%, respectively. The corresponding area-under-the-curve (AUC) scores for the central retinal vessel trunk and its branches were 0.89 and 0.90, respectively, higher than those obtained with RNFL thickness alone (reported AUCs range from 0.74 to 0.80).
“We used the complete OCT volume and the 3D structure of the central retinal vessel trunk and its branches to demonstrate its diagnostic capabilities,” the researchers noted in their paper. “We did not restrict the network to only track the location of central retinal vessel trunk or changes in the blood vessels in the frontal/en face view, but allowed it to discover novel structural configurations by analyzing the 3D structure of the glaucomatous and non-glaucomatous central retinal vessel trunk and its branches.”
While the team has good data showing the diagnostic merit of neural networks for detecting glaucoma, this novel way of interrogating the CNN to specifically deal with the vasculature shows that there is a wealth of information held in this vascular tissue itself, without even considering the neuroretina. However, it is currently difficult to assess whether central retinal vessel trunk nasalization would be expressed similarly (i.e., with the same structural characteristics) in both myopia and glaucoma, and further work is warranted.
“The paradigm introduced in this study has many potential clinical applications and may help increase diagnostic accuracy, predict future patterns and possibly impact prognosis of patients,” the study authors concluded.
Panda SK, Cheong H, Tun TA, et al. The three-dimensional structural configuration of the central retinal vessel trunk and branches as a glaucoma biomarker. Am J Ophthalmol. March 2, 2022. [Epub ahead of print]. |

